September 24, 2020
How can the Interoperability of Cloud Solutions Improve Patient Outcomes?


Michelle O'Brien, Head of Strategy
By giving health professionals easier access to patient data using the cloud, we can improve patient outcomes with less administration.
This article is the first of my series that looks to demystify and clarify the benefits of adopting Cloud solutions for healthcare. I hope this series will help save you time wading through and comprehending some of the overly technical information that is out there.
In this article I discuss how this is possible, now, thanks to how interoperable cloud systems are when exchanging health information.
We hear the term Interoperability a lot but what does it really mean in a healthcare context?
Often people are unsure what I mean when we talk about interoperability and health information exchange. What we really mean is delivering systems that allow all healthcare providers, across the healthcare continuum, access to a near live view of the patients’ longitudinal health record.
Unfortunately, many of our legacy, server based systems, which around 95% of GP’s still use, keep a patients longitudinal record in a server. As a result information is siloed from other parts of the healthcare system. If the patient only ever goes to one GP over a lifetime, then this may not be a major issue.
However, if the patient is in an Aged–Care facility, moves to a new state or unexpectedly ends up in the ED, this means the new healthcare provider has no visibility of the patients’ clinical history. This adds significant clinical risk when treating a patient, especially when the patient cannot communicate their clinical history as is often the case.
A detailed example…
An example of how our currently disconnected health system impacts on patient outcomes is a palliative care patient in an Aged-Care facility. In this scenario a patient may need shared care, requiring their medical information being accessed by:
- Their GP
- Aged care provider
- Hospital
- Specialist
- Psychology and other allied health
- Mental Health support
- Private health insurer
- Family members
- The Patient/Carers
- Ambulance services
That is 10 potential stakeholders, who may all need access to some, or all, of the clinical record.
The reality is that in an acute or urgent situation a patient’s data does not move with them; instead each stakeholder has their own piece of siloed information. Transmitting that data to those who need it is currently time consuming and laborious, due to the use of outdated technology like fax, printers, couriers, mail and secure messaging. It’s as if we give each stakeholder a single jigsaw piece, then expect them to know what the completed image is.
If this is how things are done currently – why does this matter?
This is a good question, and one which, for many in healthcare, has an uncomfortable answer. This siloed approach to patient data matters because it impacts on patients care and health outcomes.
If we go back to our palliative care patient in an Aged Care Facility, not understanding their history can lead to patients being unnecessarily transported to an Emergency Department without anyone reviewing their wishes. They find themselves in unfamiliar surroundings, with clinicians who have little background on their condition.
This outcome is distressing for everyone. If the entire care team had a view of the patients record, including their end of life wishes, outcomes for the patient would be so much better. This scenario highlights two main problems:
Problem 1: The administrative burden
The infographic below highlights some of the current challenges facing clinicians trying to manage the care of a patient. As you can see the process is stressful, time consuming and very administrative.
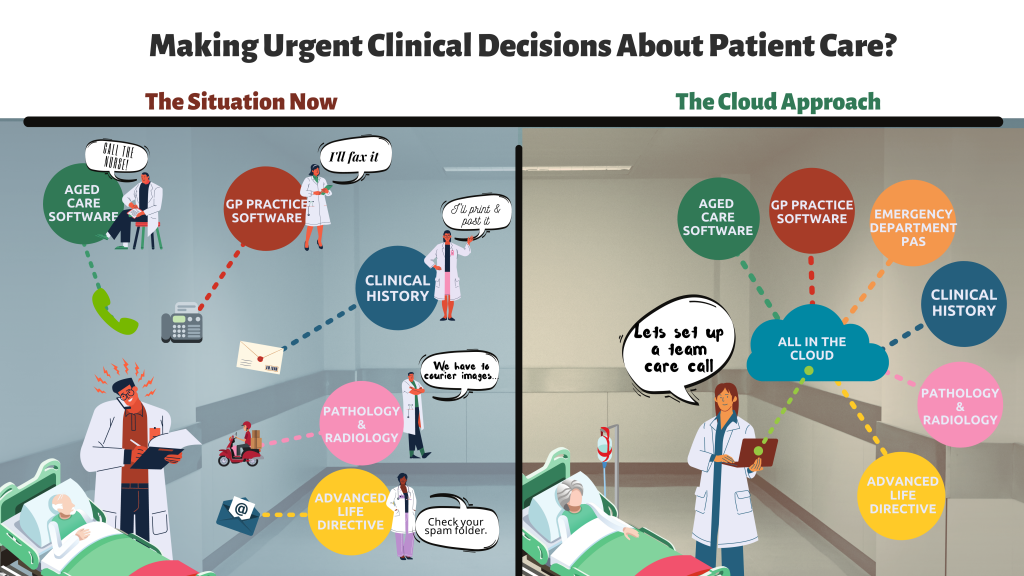
The reality is that this slow and expensive process is neither sustainable, nor acceptable for our patients. We need to find a way to manage these administrative costs through improved access to patient medical information for everyone in their treatment circle.
Problem 2: The risk to patient safety due to lack of information
The second problem is the inability to share patient data across the health system. As the patient moves between primary, acute, community and virtual settings, their risk of an adverse event increases. This is because without a complete view of the patients’ longitudinal health record clinicians are flying blind. So how can cloud systems solve the interoperability challenge?
All the problems I have mentioned can be fixed. However, it will take time for healthcare providers to understand the value of Cloud and adopting modern healthcare standards to achieve interoperability.
Our vision for the future is that all healthcare professionals will use Cloud systems. This will allow them to log in anywhere, from any device, and directly access their patient’s information.
In summary
The concept of shared, virtual, and immediate multidisciplinary team care has the potential to significantly reduce administrative costs. More importantly it can improve health outcomes through the way we manage chronic disease and mental health, and provide health and social care to our ageing population, whether they are in Aged Care facilitates or in the home.
Ultimately it is the patient who will benefit the most from Cloud technology and interoperability, thanks to the the ability to have their clinical record travel with them no matter where they are in the health care system.
Michelle O’Brien, who is based in our Sydney office, is Head of Strategy here at MediRecords.





