June 2, 2022
Taking the pulse on
digital health

MediRecords attended a packed Digital Health Festival in an icy Melbourne on 31 May and 1 June. The conference was the largest face-to-face event since the pandemic and attracted international speakers and delegates from across Australia.
A recurrent theme was that telehealth has been normalised during the pandemic and is now an everyday tool for doctors and specialists. But while digital and virtual care technology is widely used, too many systems still don’t share information and healthcare professionals are fed up with having to use multiple, disconnected products.
Here are some snapshots from the festival:
Australian Digital Health Agency CEO Amanda Cattermole said the agency remains committed to a connected healthcare system through which data passes, “seamlessly, safely and securely”. Ms Cattermole said a new National Digital Health Strategy is imminent and that the ADHA has three key roles:
- Creating a collaborative environment that accelerates adoption of digital technology, including stewarding and supporting state government initiatives.
- Building and providing ‘infrastructure glue’ that is FHIR enabled, web-based and includes a new health API gateway to national digital health systems, due by the end of 2022.
- Co-designing a governance framework, or the ‘guardrails’ for a national healthcare interoperability plan.
ADHA projects under way also include:
- a national digital children’s health record, replacing state-based systems
- a framework for sharing population health data ethically and securely
- a national digital imaging platform for diagnostic medical imaging, and
- a My Health Record mobile app.

My Emergency Doctor founder and Medical Director Justin Bowra explained how virtual ED doctors help improve patient flow and reduce clinical risks at hospitals and urgent care centres. Dr Bowra said MED clinicians conduct case conferences via video calls, including reviewing the status of patients waiting in ambulances. The case conferences enable patient flow decisions that reduce ED wait times, such as advising that patients can go direct to theatre. The service also provides clinical decision support and mentoring to on-site doctors and an auditable recording of all interactions.
Caligo Health Managing Director Dr Amandeep Hansra said the COVID-19 pandemic had catapulted digital health innovation forward by at least a decade, creating created consumers who are actively engaged in their care and demand access to and control of personal data. The pandemic had also created a mountain of data — 30% of global data comes from health — that could be the foundation for scalable analytics and AI-driven businesses.
e-Health Queensland Health Deputy Director General Damian Green walked festival goers through the Sunshine State’s digital strategy, emphasising the importance of human-centered design and delivering equitable healthcare access for First Nations peoples and diverse communities. Mr Green said clinicians were required to work with too many products and ‘system sustainability’ would necessitate fewer systems with the requisite data for better decision making. He said safety was at the heart of all digital investment decisions and told vendors, “if you can show you are going to improve outcomes, then talk to us.”
Victorian Department of Health Chief Digital Officer Neville Board placed patient safety as the destination for the Garden State’s digital health roadmap. Mr Board said reducing risks to patients caused by paper-based processes was a major priority and showed how e-prescribing significantly reduces risks of medication errors. Victoria has also committed to a Health Information Exchange that enables interchange of information between all hospitals.
Neville Board placed patient safety as the destination for the Garden State’s digital health roadmap. Mr Board said reducing risks to patients caused by paper-based processes was a major priority and showed how e-prescribing significantly reduces risks of medication errors. Victoria has also committed to a Health Information Exchange that enables interchange of information between all hospitals.
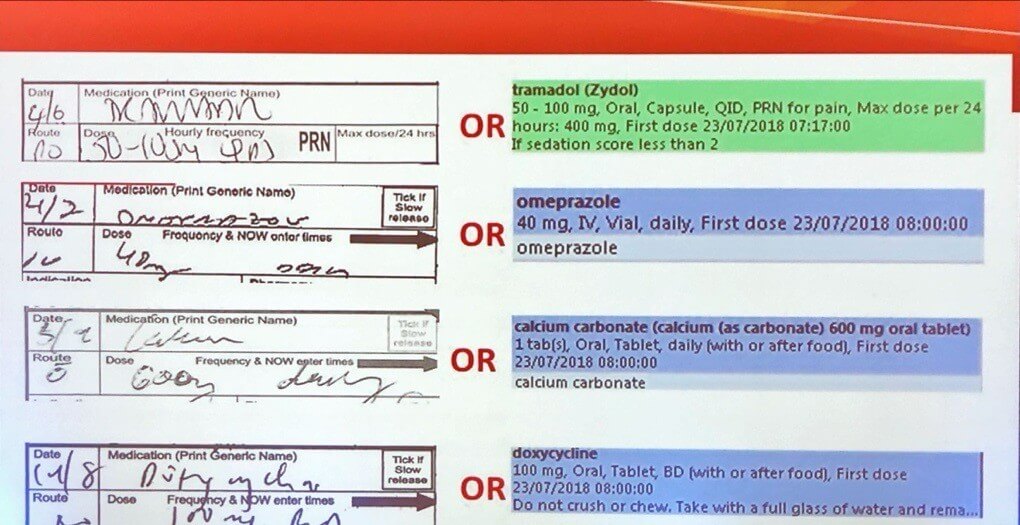
Victorian Chief Digital Officer Neville Board highlights the risks of handwritten medication notes.
Alcidion CEO Kate Quirke said procurement processes in Australia were a deterrent to innovation and that many Proof of Concept projects did not proceed to implementation because contractual requirements were too onerous.
Former Deputy Chief Medical Officer Dr Nick Coatsworth said healthcare start-ups need to be thoroughbreds capable of going the distance, rather than flashy unicorns. And the secret to designing an enduring product? Make sure you’re solving problems for patients and their families.
Dr Emma Rees, Founder and CEO of women’s healthcare platform Femma, said health care should not cease when a patient leaves the room and be suspended until a follow-up appointment. Dr Rees said “the future of healthcare is a hybrid model” where patients have clinically curated, individual management plans and on-demand access to education materials and nutritional, exercise, mindfulness and yoga programs.
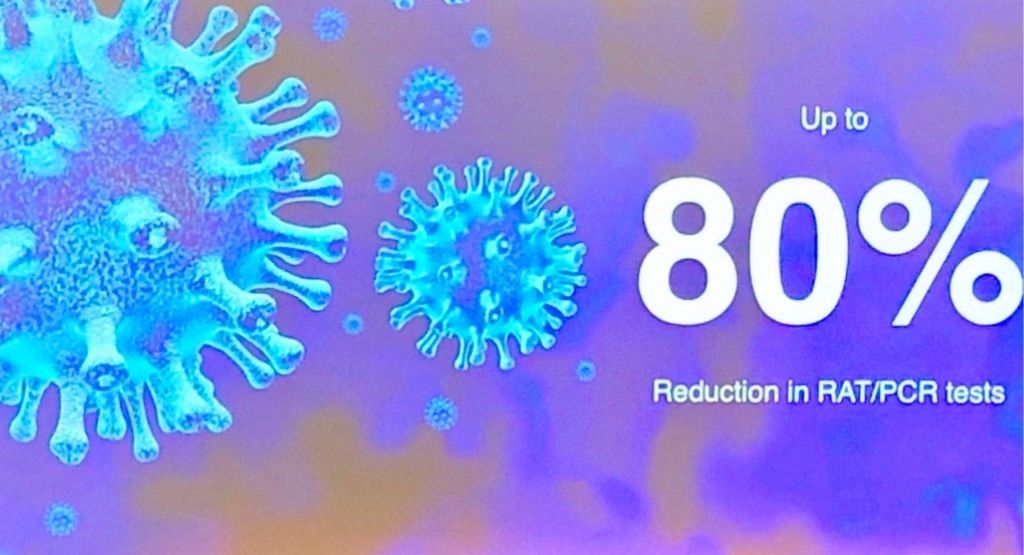
Image courtesy of ResApp
Australian start-up ResApp has developed a digital diagnostic app for respiratory illnesses, available on mobile devices. The ResApp tool listens to a patient cough five times and then sends a report direct to a GP. ResApp CEO Dr Tony Keating said trials in India and the US had shown a high level of accuracy in diagnosing COVID-19. Using the app for initial diagnosis could make up to 80% of RAT and PCR testing unnecessary, bringing immediate benefits for patients, cost savings for governments and environmental benefits.
The Global Healthcare Lead for Zoom, Ron Emerson, said research by a leading US healthcare provider had shown that 70 per cent of patients attending at urgent care facilities could be safely seen by a virtual health care clinician, helping to relieve pressures on overcrowded hospitals. Zoom is now being used by prestigious US healthcare organisations, including the Mayo Clinic, Johns Hopkins and New York Presbyterian hospitals.







