July 9, 2024
What's happening in health?

As one of the biggest industries on the planet, there’s always something happening in healthcare. Here’s what has captured our attention recently.
Industry news
Private hospitals are facing tough times as costs of doing business keep rising while a major source of their revenue – private health insurers (PHI) – are seen to be holding tight to profits. The ill-will between PHI and private hospitals is best demonstrated by the battle between the St Vincent’s group and NIB, which is at breaking point.
Suggestions of a crisis in the private hospital sector are underlined by key players co-operating with a Federal Government review. Health Services Daily reports that, “79 facilities — including day surgeries, endoscopy centres, private hospitals, wound care centres, cosmetic surgery centres, dental centres, respiratory and sleep disorder clinics, dialysis clinics and mental health centres — have either closed or revoked their declaration as a private hospital since 2019”.
Internationally, post-pandemic use of telehealth has fallen and major retail chains who leapt into healthcare are back-pedalling. American companies Walmart and Walgreens winding back their health businesses (see What retail titans might do next on health care (axios.com)), makes us wonder how Healthylifeis going for Woolworths, locally.
The pressure to be profitable means most hospitals are searching for ways to reduce the costs of delivering care. Managing patients in their own beds may be cheaper than hospital beds and so the cash-strapped UK National Health Service has committed to scaling up virtual care.
If the NHS needs a success story to use as inspiration, the ever-innovative Cleveland Clinic is hailing its acute hospital care in the home program a success for patients and staff, while acknowledging further improvements are possible. For details, see Lessons from Cleveland Clinic’s 1st year of ‘hospital at home’ (beckershospitalreview.com).
Melbourne’s Austin Hospital has also committed to virtual wards as business as usual, particularly for cardiac and haematology patients.
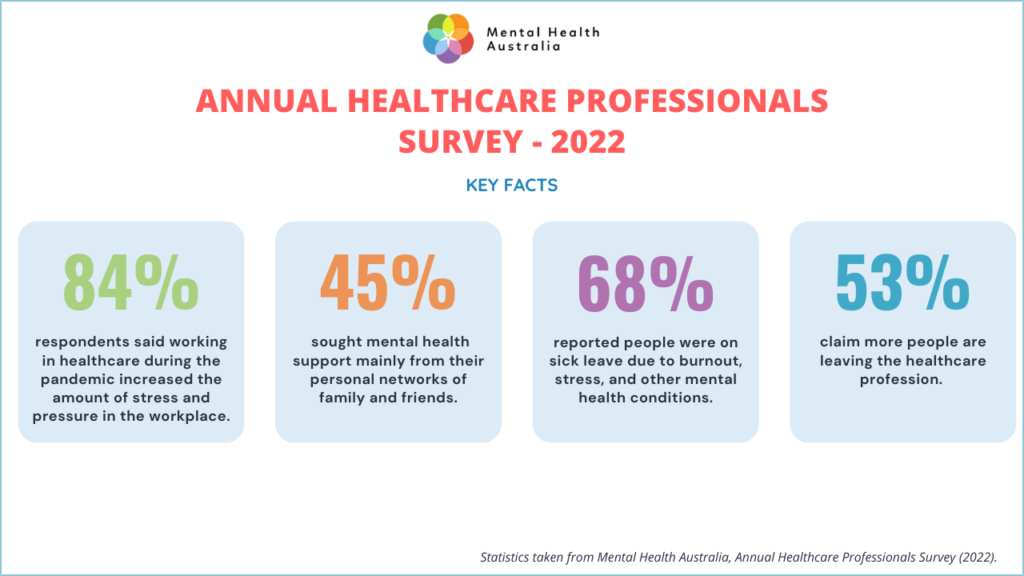
And the Federal Government is funding virtual careto chip away at a barriers to accessing mental health inpatient care, (partly caused by a shortage of accessible psychiatrists).
Keeping it real on artificial intelligence
Investors seeking share-market alchemy remain bullish on Artificial Intelligence while potential end users want ethical, regulatory and security assurances to precede introduction of these potentially very useful new tools. The American Medical Association offers sensible tips on technology adoption here: In the push for AI in health care, avoid EHR rollout mistakes | American Medical Association (ama-assn.org)
As to the smorgasbord of AI news, here is an aperitif:
- Stroke recognition in ambulances: Mobile face screening tool detects stroke ‘in seconds’ | MobiHealthNews
- Reducing alert fatigue for clinicians: How 5 health systems reined in patient portal messages (beckershospitalreview.com)
- Predicting patient deterioration to enable earlier intervention: Real-Time AI Alerts Reduce Patient Deaths by 43%, Mount Sinai Study Finds (hitconsultant.net)
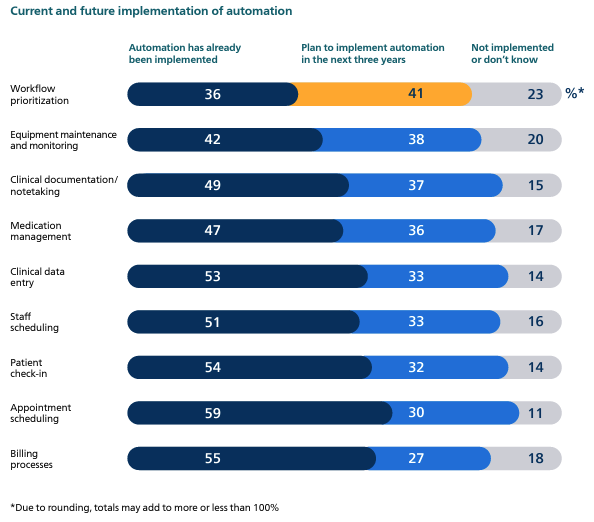
- Automation most likely where it reduces burnout: philips-future-health-index-2024-report-better-care-for-more-people-global.pdf
- Will AI replace doctors? If a doctor and an AI app both have 95% accuracy, what’s the difference? | Healthcare IT News
We're all healthcare consumers
We also keep a close watch on consumer health news, in the interest of all of us avoiding hospitalisation. Here are some insights aimed at keeping our engines running:
Evidence is mounting that good gut health boosts mental health and ability to handle stress. Stress: Could a healthy gut microbiome make you more resilient? (medicalnewstoday.com)
Multivitamins, however, might only contribute to expensive and colourful urine. Another Study Finds No Life-Extending Benefit From Multivitamins (healthday.com)
In other product news, the old advice (or excellent marketing) that taking aspirin reduces risk of heart attack appears to have been debunked – unless you have previously had a stroke or heart attack. American Adults Warned Over Aspirin Use Despite Risks – Newsweek
Stanford University research, published in the journal Nature Medicine, has identified six different types of depression, which has implications for better treatment and management of mental ill-health. 6 types of depression identified in Stanford study | CNN
And there are clear reasons to avoid COVID19 because the long form of the illness is particularly nasty. Report: More than 200 symptoms tied to long COVID | CIDRAP (umn.edu)
The last word
Police, prisons and hospital emergency departments are often the professionals most likely to be dealing with people experiencing acute mental ill health. Here’s a good news story of how technology and faster access to treatment can successfully divert people from EDs and custody – https://www.healthcareitnews.com/news/outfitting-police-telehealth-ipads-mental-health-program-saves-government-62m?