Throughout July we ran a survey for users of Medical Practice Management Software, like MediRecords. The aim was to listen to, and learn from, both our own users and those who use alternatives.
In this article we have summarised some of the more interesting insights around:
- the impact of COVID on doctors
- the working environments of clinicians
- what users want from practice management software, and
- How important Telehealth features are to clinicians.
If any of this sounds interesting, then please read on! But before we get into it, we would like to say a big thank you to all who took part in the survey.
As with all survey data, the stats can often be interpreted in many ways. If you have any insights or explanation for what we found in the survey, we would love to hear from you via marketing@medirecords.com.
About the Survey & Audience
Our survey was delivered to GP clinics via fax, email and through The Medical Republics e-newsletter. Whilst the survey was open to clinicians, practice managers, nurses and business owners, most respondents primarily identified as clinicians.
We ran our survey throughout July, which ended up being an interesting time. The initial explosion of conversations around Telehealth had begun to quieten down (more on this later), whilst Victorians began seeing lockdown restrictions gradually being enforced as they experienced their ‘second wave’.
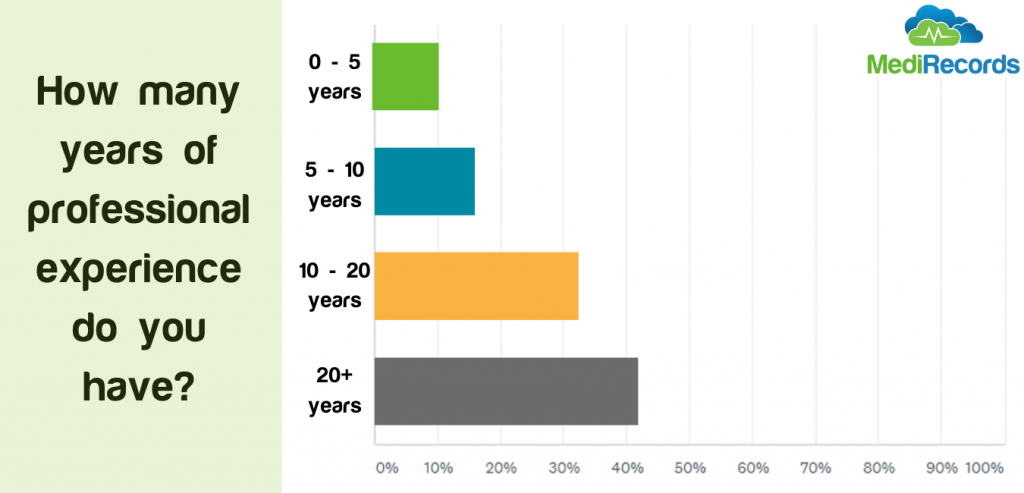
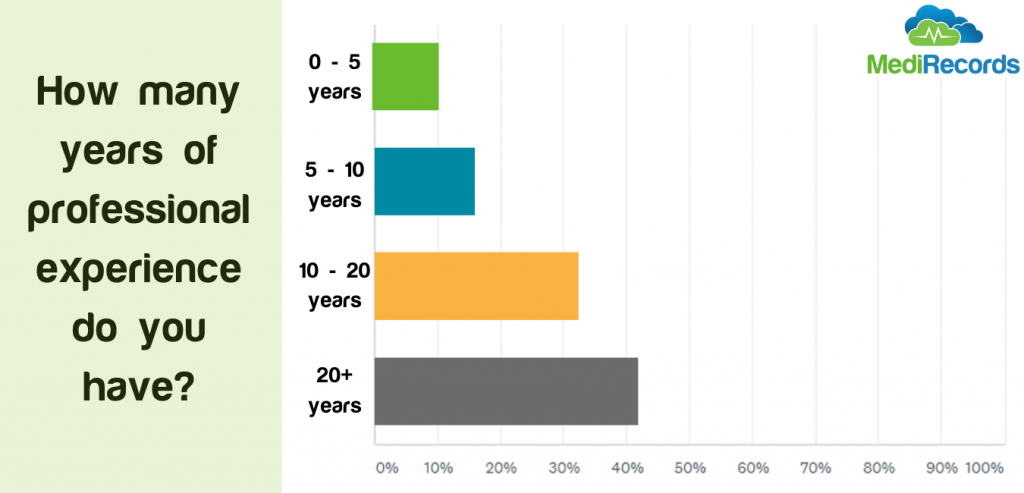
One noticeable skew was that the audience had a significant amount of professional experience, with over 40% having over 20 years in General Practice, which is worth bearing in mind as you read this article:
GP’s Working Environment
We were keen to understand how GPs tend to work, as this allows us to better understand how MediRecords can be as useful to clinicians as possible.
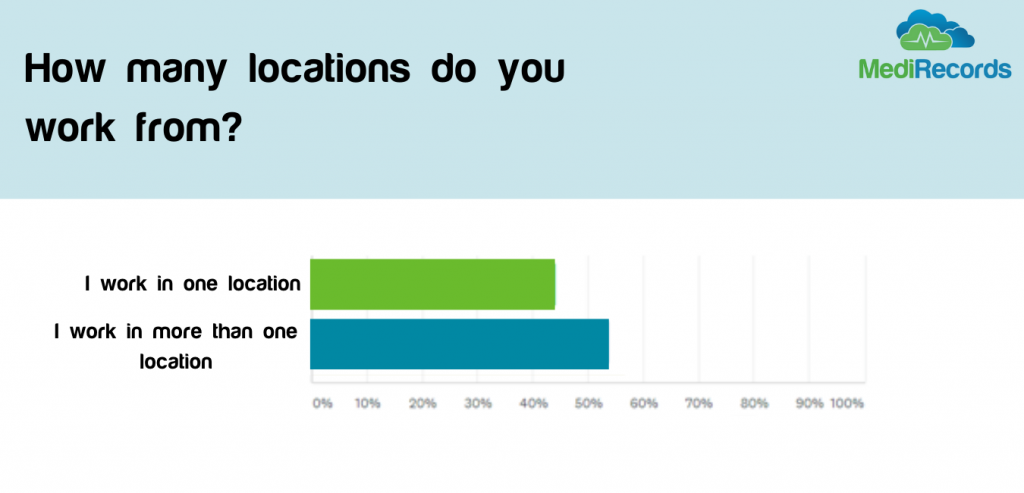
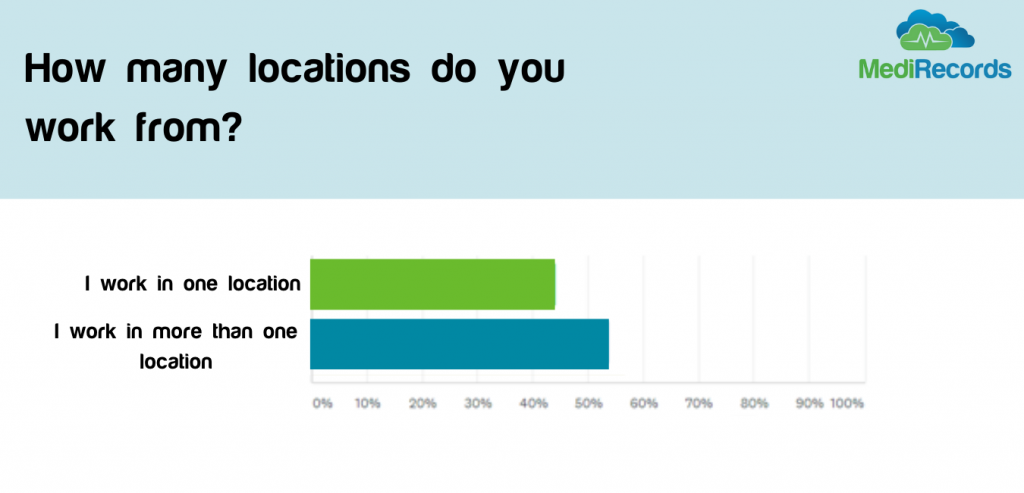
We found GP’s were split fairly evenly between those who work in one location, and those who work across multiple locations. What is not clear if this means they work across multiple practices, or often from home, something which could be influenced by the current pandemic.
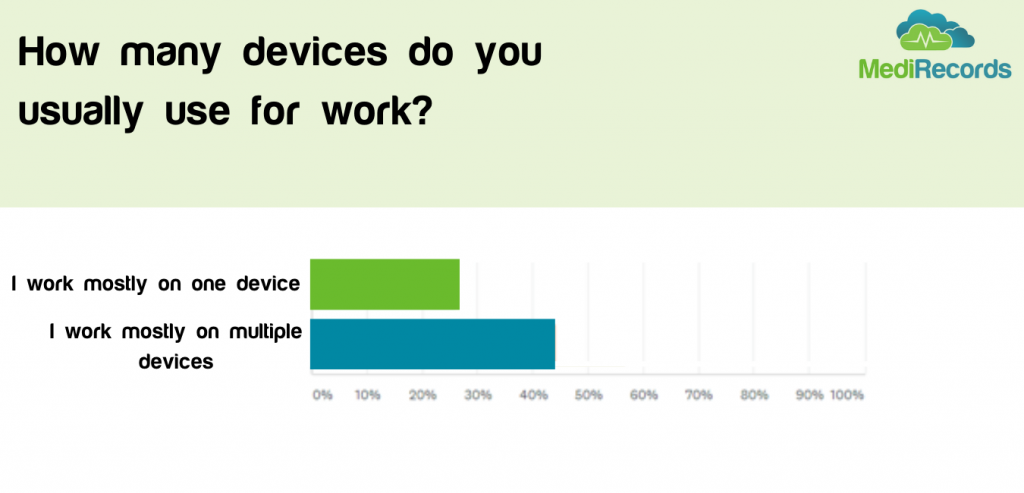
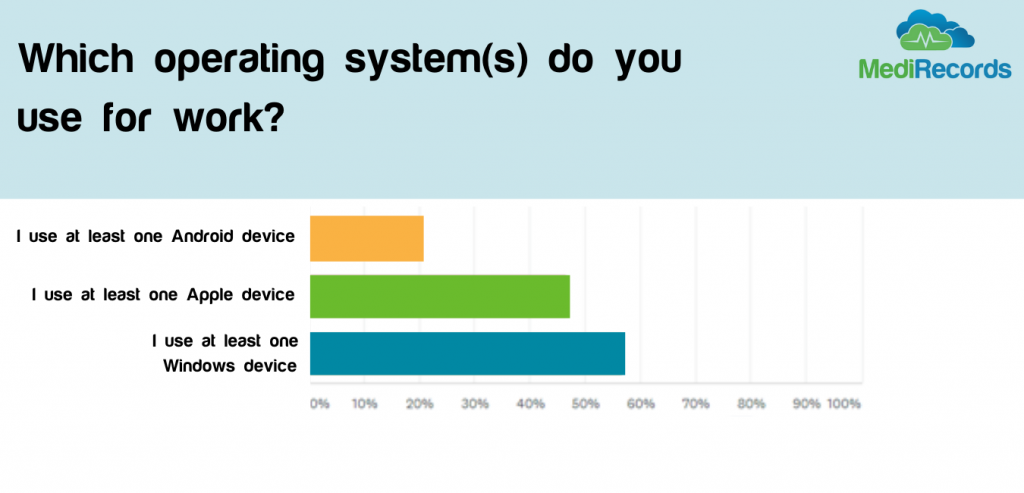
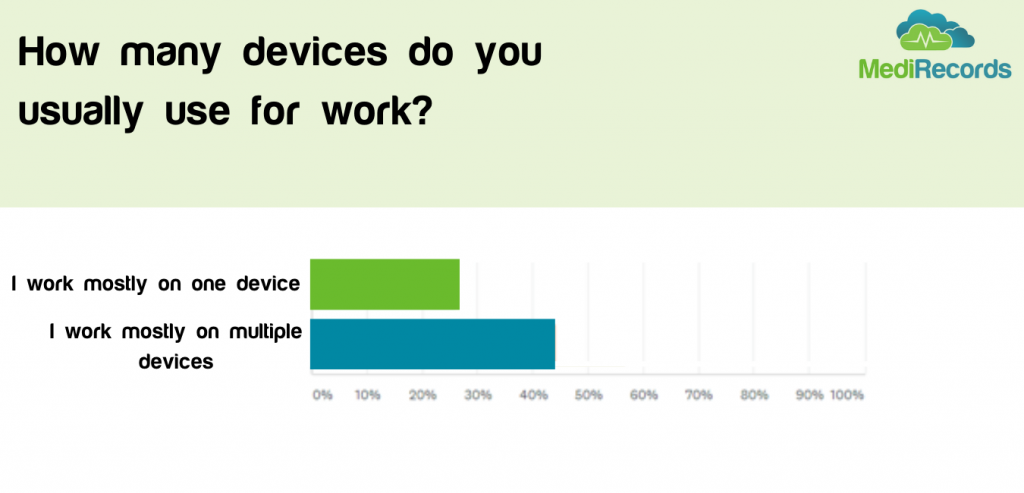
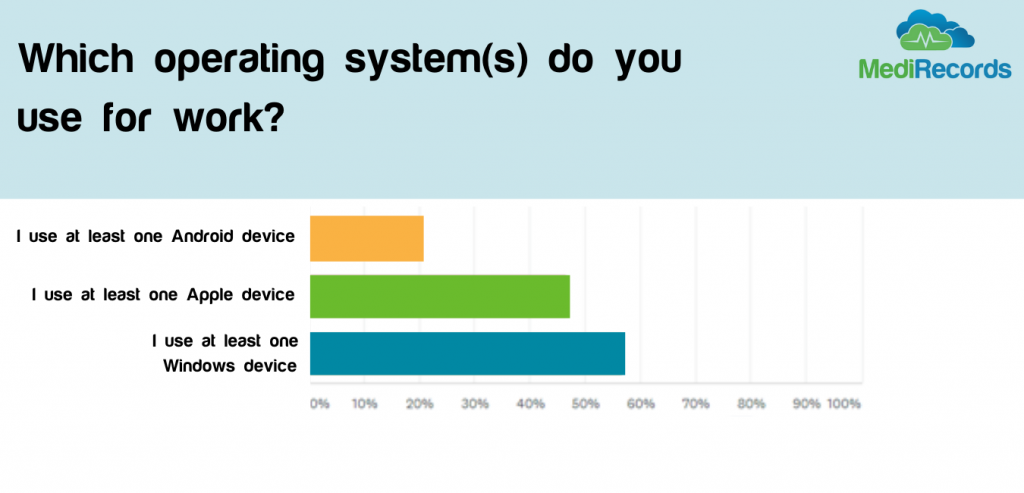
Far more clinicians work on multiple devices rather than one, which us unsurprising given our consumer habits across phones, tablets and computers. It is particularly interesting for practice management software however, as ease of working across devices and locations is very difficult on server-based solutions such as Best Practice and Medical Director, compared with cloud solutions like MediRecords.
It was interesting to see that almost as many people use Apple products as do Windows, again something that could make browser-based software more appealing to ensure consistency of experience and usability for GPs on whichever device they use.
Preferences for practice management software
We asked our GP respondents a lot of questions about their preferences are for practice management software. This information is best summarized in the two questions:
- What do you like about your Practice Management Software ? And…
- What do you not like about your Practice Management Software?
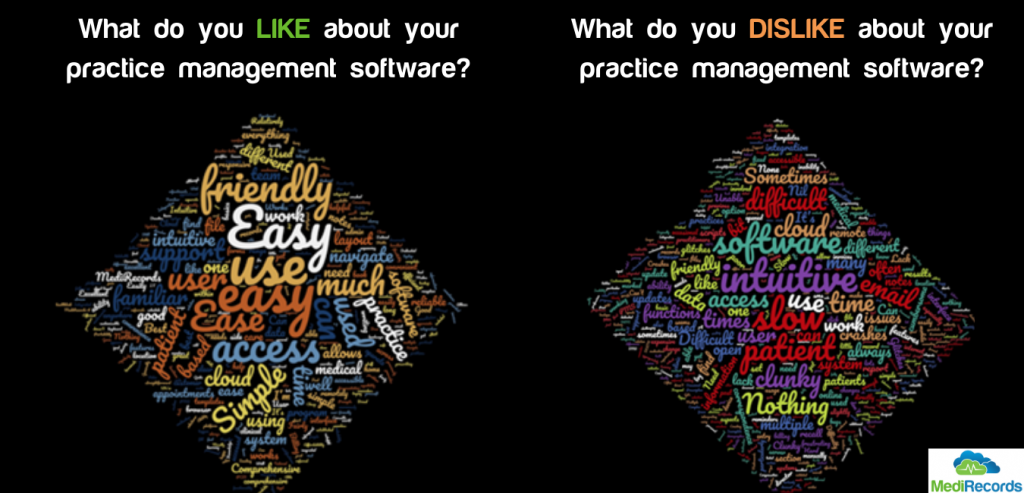
Surprisingly, the same sort of answer was most popular for both questions – Usability!
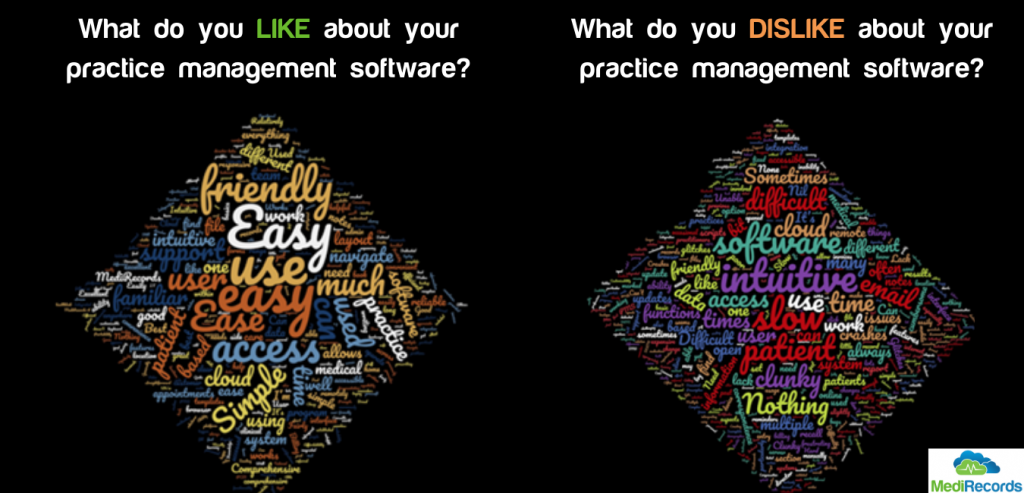
It can be easy to get lost in specifications and functionality lists when choosing Practice Management Software, but what this shows us all is that, fundamentally, it means little if the platform is not easy for clinicians to use. We suspect this will also be what drives most day to day frustrations users have with their current software.
(By the way, we think this is great news given the positive feedback we have had on MediRecords from our users. If you are struggling with usability there is a solution!)
So, are clinicians looking for something better?
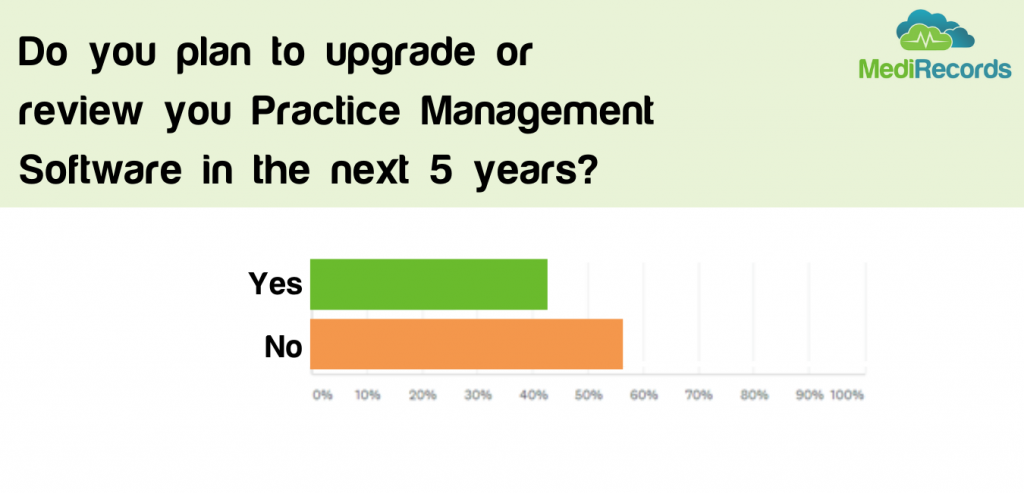
We then asked if clinicians were planning on reviewing or upgrading their software over the next five years. Only 40% of respondents said they would consider doing so.
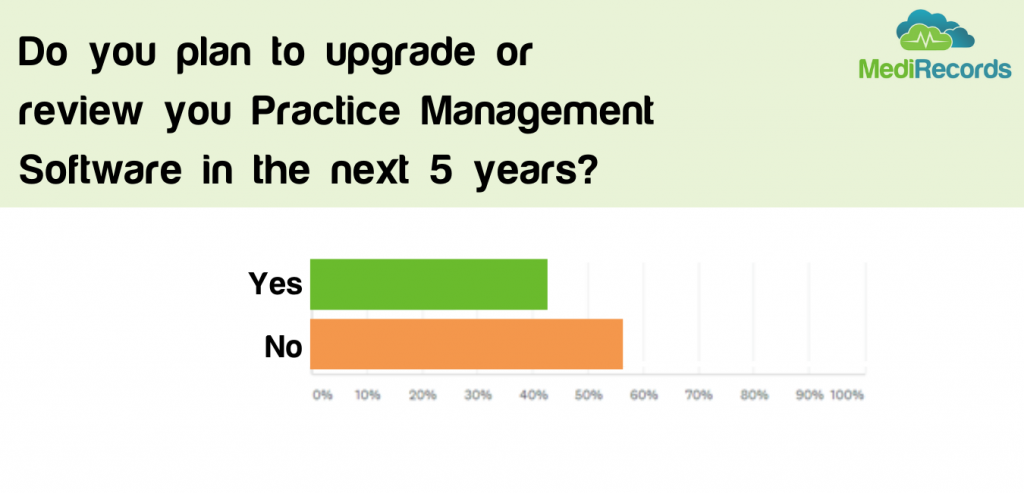 Many in the healthcare tech space may find this disappointing, but we believe it shows us the wider trend of reluctance to adopt and change with new technologies. Whilst many may be heralding a silver lining of COVID to be increased adoption of technology, the results suggest this mindset change will not happen overnight – even if pushed by a major event such as COVID.
Many in the healthcare tech space may find this disappointing, but we believe it shows us the wider trend of reluctance to adopt and change with new technologies. Whilst many may be heralding a silver lining of COVID to be increased adoption of technology, the results suggest this mindset change will not happen overnight – even if pushed by a major event such as COVID.
If clinicians are still reluctant to change, what does this mean for Telehealth adoption?
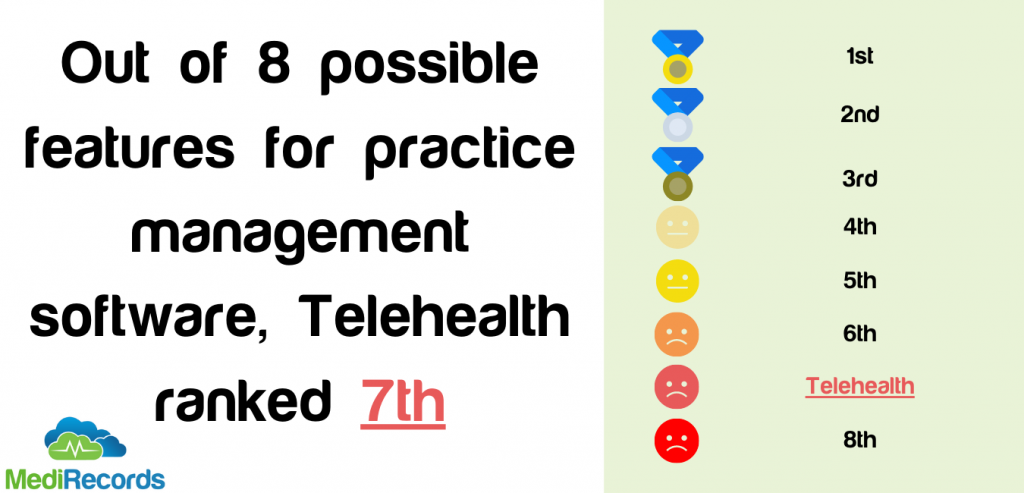
We asked respondents to rank features in terms of the importance to them when choosing practice management software. Whilst we won’t be sharing the full results of this (hopefully you can understand, we want to keep some knowledge to ourselves!) what was surprising was that Telehealth was the second least important feature to the GPs we asked.
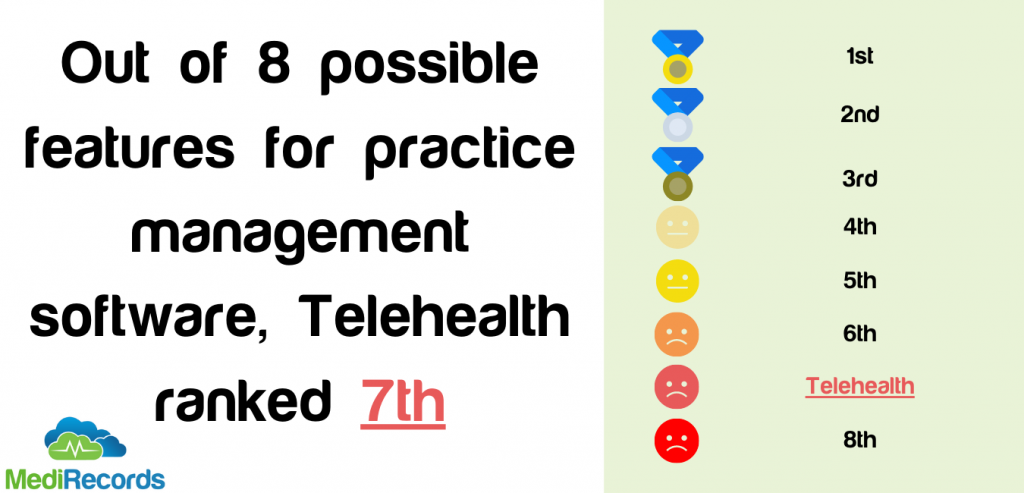
The timing of the survey may have had something to do with this. Whilst in the earlier days of the pandemic many GPs were trying to figure out how to incorporate Telehealth into their daily workflow, by July Telehealth MBS items had been live for over a month, with GPs finding that using the telephone was an easier, more familiar solution in the short term.
Again, this may reflect the reluctance of many to adopt new technologies, even if these technologies lead to better experiences for patients. We can see the benefits of telehealth via remote monitoring via projects such as Spritely’s recent trial in retirement villages in Christchurch, but clearly there is more work to be done to help clinicians see if there is a benefit for them.
So, what do clinicians want from their PMS?
Finally, we asked what GPs wished their PMS could do that it does not already.

The results here were less clear, with 27% of people wanted a feature specific to their practice’s requirements, and a further 20% wanting an integration with a specific other service.
This shows how personal and bespoke the needs of many practices are, and how software such as MediRecords must not only be flexible for different workflows, but also responsive to users when they need new feature.
Again, usability came up, this time as something that respondents wish their PMS offered. Given the large share of the market enjoyed by traditional solutions such as Medical Director and Best Practice, perhaps this reflects the need for clinicians to look at some of the newer, easier to use options that are out there.
Personally, we think MediRecords fits the bill perfectly! If you would like to find out more you can contact support@medirecords.com, book a demo, or enjoy a 30 day free trial now.
About the Author
Andrew Dyson is our Digital Marketing Lead here at MediRecords, and managed this latest survey. Prior to joining MediRecords he has worked on marketing projects, including in depth market research, for some of the largest employers in the UK.

















 Many in the healthcare tech space may find this disappointing, but we believe it shows us the wider trend of reluctance to adopt and change with new technologies. Whilst many may be heralding a silver lining of COVID to be increased adoption of technology, the results suggest this mindset change will not happen overnight – even if pushed by a major event such as COVID.
Many in the healthcare tech space may find this disappointing, but we believe it shows us the wider trend of reluctance to adopt and change with new technologies. Whilst many may be heralding a silver lining of COVID to be increased adoption of technology, the results suggest this mindset change will not happen overnight – even if pushed by a major event such as COVID.