May 22, 2024
The power to prescribe:
Who should have it?

A couple of weeks ago at a media conference, a Pharmacy Guild representative was photographed wearing a stethoscope over his white smock. The image triggered an adverse reaction among GPs; some asked how a pharmacist would use the instrument, others whether the event was a costume party.
The heated response suggests the national conversation over whether pharmacists should be able to extend their limited prescribing rights is gaining heat, rather than cooling. So what’s the debate all about? Let’s look at the key parties and what they say is at stake.
Party one: Pharmacists (represented by The Pharmacy Guild of Australia and Pharmaceutical Society of Australia)
Many pharmacies already offer vaccination services and support for chronic disease management. Trials have been conducted in several states, focused on providing assistance to people with conditions such as urinary tract infections (UTIs).
Pharmacists believe they can do even more to assist Australians who need help with common conditions and will be coming to them to collect medications anyway.
Backed by the Queensland government, the Guild initiated the North Queensland Pharmacy Scope of Practice Pilot, pencilling it for December 2023 and kicking it off in April 2024. Under the pilot, conditions pharmacists can now treat include acne, hay fever and eczema. For the full list, see About the pilot | Queensland Health.
The Queensland Government has since moved to make the North Queensland pilot statewide.
Party two: Governments
Governments are trying to solve a supply and demand problem. It’s hard to get a GP appointment just about anywhere — and generally harder the further you are from a state capital.
Queensland Premier Steven Miles said: “Our Government is committed to making sure Queenslanders can access good quality healthcare, no matter where they live across the state.
“We know our hardworking pharmacists are more than capable to deliver these services – for common health conditions – and divert people away from our emergency departments and GPs.
“I am really proud that Queensland is leading the nation with this initiative.”
Queensland Health states: “Pharmacists are highly qualified and trusted members of our healthcare teams. Providing pharmacists with additional clinical training and supporting them to practice to their full scope, will enable them to help and support their local communities.”
Party three: General Practitioners (represented by the Royal Australian College of General Practitioners (RACP) and Australian Medical Association)
Doctors say that medications cannot be safely prescribed without a holistic, longitudinal view of the patient’s medical history, as best understood by their usual GP. They say the pilot puts vulnerable people at risk and that a previous trial allowing pharmacists to prescribe antibiotics for UTIs led to incorrect diagnoses and serious conditions going untreated, increasing overall healthcare costs.
Party four: Healthcare consumers (represented by you and I)
While most people prefer a long term relationship with a GP who knows you and your family, getting an appointment when you need it isn’t always easy or affordable. Some people go to hospital emergency departments (or virtual versions) for free help.
Other consumers are opting for convenience, using telehealth providers that offer quick access to scripts and more, but might not have time to hear your health history, (if you can remember it). For this group of consumers, getting help from the pharmacy you’re going to anyway, may be a no-brainer. However, the services are not free. Fees of up to $55 per pharmacist consultation may limit take-up.
Those with multiple or complex conditions are likely to have to wait for the next available appointment with their GP and hope for a cancellation to get in sooner.
Sparring partners
Back in March, the Medical Software Industry Association promised a ‘ding dong battle’ between the Guild, the RACGP and government, placing three key representatives on stage together in Melbourne.
Pharmacy Guild Victorian president Anthony Tassone said the prescribing issue was not about “pharmacists being GPs. It’s about pharmacists being the best professionals they can be…. solving problems for patient benefits.”
RACGP past president Dr Karen Price said she was concerned about the ‘taskification’ of general practice, which hindered longitudinal care. Dr Price said it can take 45 minutes to explore a patient’s medication history before writing an appropriate script. She said a UTI is a “retrospective diagnosis where there may be other issues that can’t be picked up by a pharmacist”.
Representing the Federal Department of Health and Aged Care, First Assistant Secretary (Medicare Benefits and Digital Health Division) Daniel McCabe said Australia faced “acute workforce challenges” and governments were trying to unlock the full potential of professionals who could deliver, “true multidisciplinary care”.
Dr Price said multidisciplinary care was great in hospitals and, while desirable, underfunded and challenging in general practice where, “the people who most need care can least afford it”.
Mr Tassone said doctors and pharmacists were all on ‘Team Patient’ but he and his peers were not rewarded for being part of multidisciplinary teams. “Are we part of the team or are we on the bench to make up the numbers?”
He said: “Patients don’t care. They care about getting care when they need it.”
It seems this conversation is far from finished.
Skin in the game
MediRecords provides secure, cloud-hosted electronic health records and prescribing functionality to healthcare professionals across Australia delivering face-to-face and virtual care.
Further reading:
Rollout begins for Australian-first pharmacy pilot – Ministerial Media Statements
What we know about Queensland’s pharmacy prescribing pilot – Medical Republic
The Pharmacy Guild Australia QLD (pharmacyfullscope.com.au)
Queensland Community Pharmacy Scope of Practice Pilot | Queensland Health
RACGP – Pharmacy pilot a ‘solution’ that would only cause bigger problems
Unleashing-the-Potential-an-open-and-equitable-health-system.pdf

























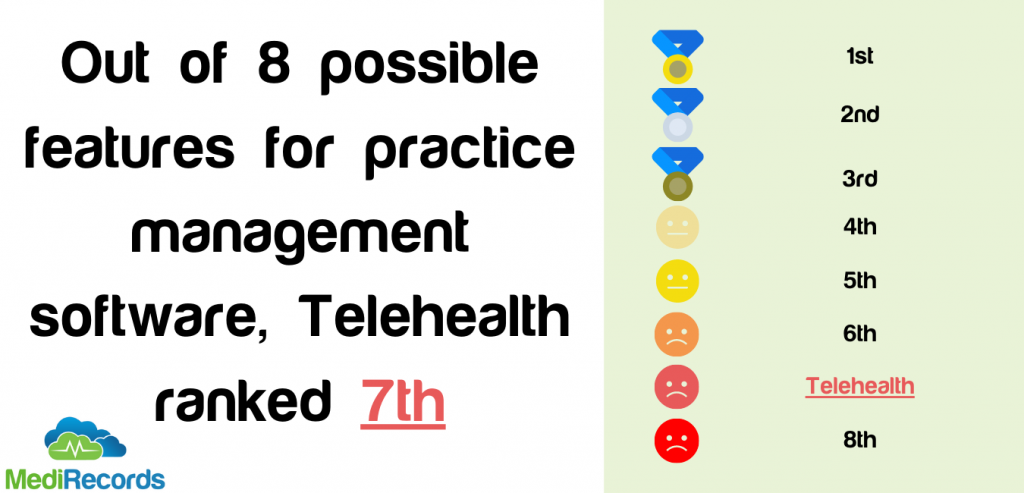
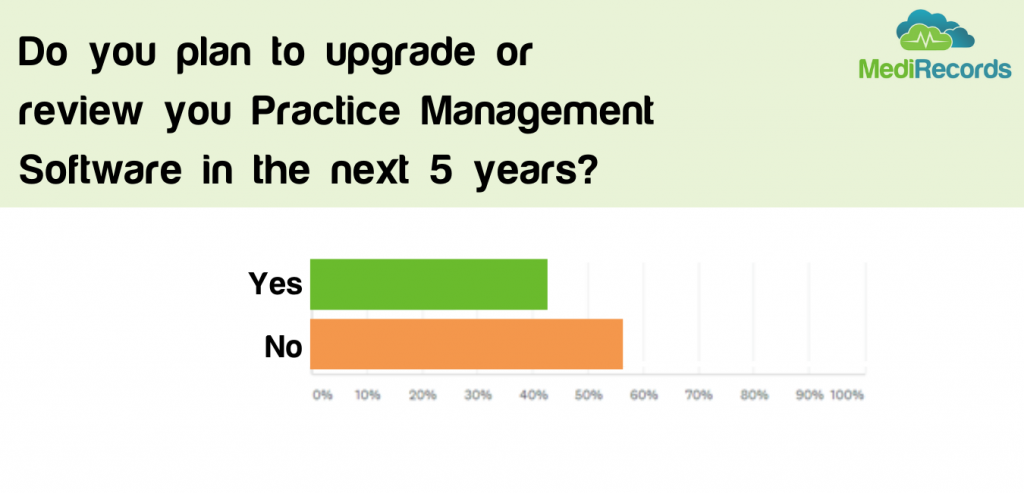 Many in the healthcare tech space may find this disappointing, but we believe it shows us the wider trend of reluctance to adopt and change with new technologies. Whilst many may be heralding a silver lining of COVID to be increased adoption of technology, the results suggest this mindset change will not happen overnight – even if pushed by a major event such as COVID.
Many in the healthcare tech space may find this disappointing, but we believe it shows us the wider trend of reluctance to adopt and change with new technologies. Whilst many may be heralding a silver lining of COVID to be increased adoption of technology, the results suggest this mindset change will not happen overnight – even if pushed by a major event such as COVID.