October 10, 2023
84% of healthcare workers
facing burnout, putting mental health at risk

On World Mental Health Day, it is timely to remember the importance of supporting the mental health of healthcare workers.
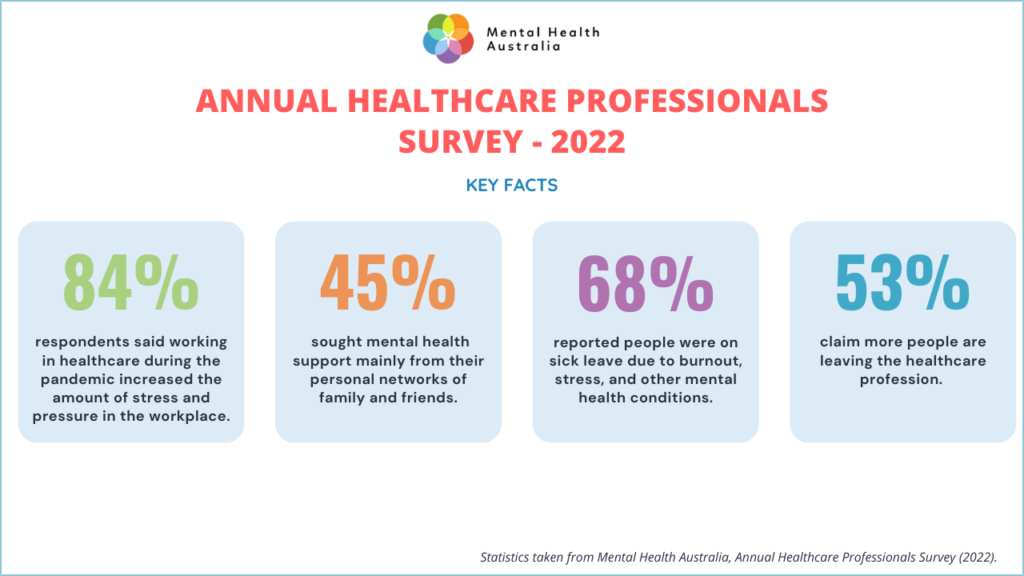
The latest data from Mental Health Australia’s (MHA) annual survey of the mental well-being of healthcare workers paints a concerning picture.
The survey found 84% of respondents reported that the pandemic’s demands lead to burnout in 2022.
The WHO describes burnout as a syndrome caused by unmanaged workplace stress. It includes feeling exhausted, negative about work, and ineffective.
Burnout is linked to a conceptualised “COVID-19 fourth wave”, alongside psychological trauma, mental illness, and economic strain, according to the US physician, Associate Prof. Victor Tseng.
Burnout significantly raises the risk of unsafe care by doctors and nurses, studies show.
In a review of 13 studies involving 20,643 doctors, “physicians with overall burnout had almost three times greater odds of making self-perceived errors,” found a study in the Journal of Patient Safety in 2022. The odds were almost identical for nurses, with burnout likely to providing poor-quality care, a separate study found this year.
One leading organisation supporting the wellbeing of healthcare professionals is the Black Dog Institute. It established The Essential Network (TEN), which aims to prevent burnout.
TEN offers practical resources , confidential personalised support and up to five free telehealth sessions.
“Every Australian has been impacted by COVID-19, but few have felt the brunt of the pandemic more keenly than health professionals,” said Black Dog Institute’s Deputy Director and Chief Psychiatrist, Professor Sam Harvey.
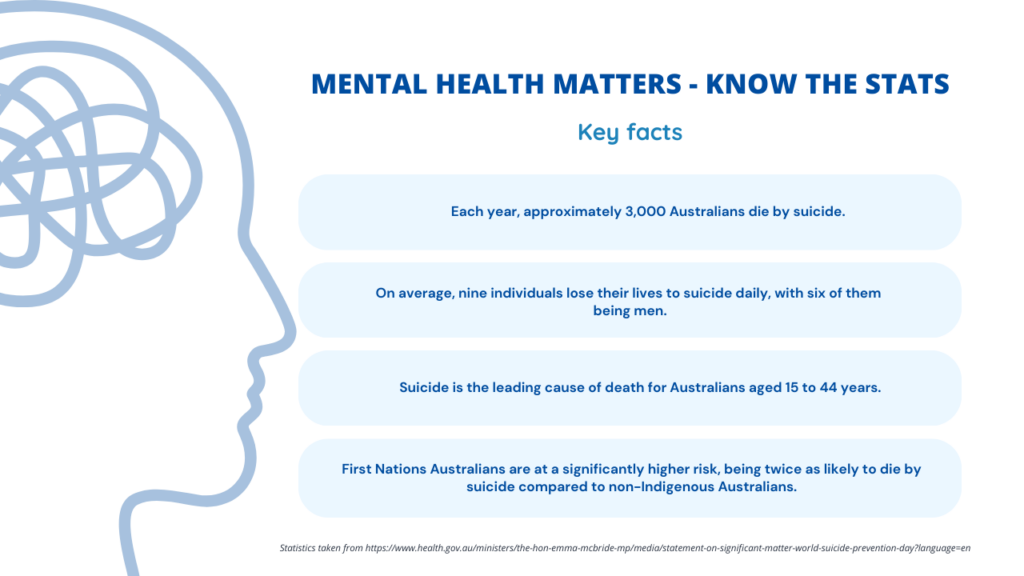
Mental Health Australia CEO Carolyn Nikoloski said that, for the first time in 20 years, Australia does not have a national mental health and suicide prevention plan. She said: “A national roadmap needs to be developed to address these concerning trends and ensure equitable access to mental health care supports for all people in Australia.”