June 17, 2024
Feeling the heat at Burning GP

MediRecords joined the sun-starved throng flocking to the Tweed for the Wild Health Burning GP conference last week.
Here are 10 takeaways from two days of robust and enlightening conversations.
1. GPs are divided on the impact of Urgent Care Centres (UCC)
Are nascent UCCs an attempt to woo voters in outer suburban marginal seats, a means to divert a few people from crowded hospital emergency departments… or an example of government spending that would be better invested in primary care? The Royal Australian College of General Practitioners (RACGP) past president Adj Prof Karen Price also pondered whether UCCs are turning away “non-urgent” patients and referring them back to their family GPs.
2. There’s a great divide between GPs and hospitals
Healthdirect Australia is trialling a way to send NSW hospital discharge summaries to GPs and patients and Queensland discharge summaries are uploaded to The Viewer … but the data disconnect between primary and tertiary care remains vast*.
Associate Professor Alam Yoosuff, the Rural Doctors Association NSW vice president, said GPs were often left in the dark about hospital outcomes for their patients.
“We don’t always know if person has died, been discharged, or been sent home with only six (tablets)… We know the system is not right. It may be better than other countries, but we know it should be even better, given what (governments) are spending.”
– Associate Professor Alam Yoosuff, the Rural Doctors Association NSW vice president
Judging by the overall vibe at Burning GP, GPs feel much of the government cash spent on shiny new hospitals could be better spent on disease prevention led by community-based primary care practitioners.
3. Workforce scaling
The RACGP warned Australia has a “whole of health” workforce crisis, exacerbated by insufficient medical students coming through, so we’re going to have to import doctors, nurses and specialists from overseas. (The ever-resilient Health Department Assistant Secretary Medicare Benefits and Digital Health, Mr Daniel McCabe, said he preferred “critical juncture” to crisis, triggering a running joke for the entire conference.)
Grampians Health Chief Strategy & Regions Officer Dr Robert Grenfell said the shortage of GPs in western Victoria was so acute he was planning based on having none. He said: “If we have (GPs) I will use them” but it was now prudent to make alternative plans.
4. Medicare misery is multiplying
Several conference panels highlighted the challenges of determining the correct, optimally reimbursed Medicare item codes for complex consultations. Mr McCabe conceded all billable items are due for review, with an aspirational goal of improving access to healthcare for people who can least afford it.
5. Telehealth – supplementary or threat?
If young and tech-savvy consumers keep opting for online access to quick prescriptions, medical certificates and more, community GPs will be left with older, sicker, more complex clients, including those with mental ill health. Whitebridge Medical Centre owner Dr Max Mollenkopf said GPs needed to understand why consumers are switching to digital health companies such as Eucalyptus and adapt fast. He said, “Our old patients who love us will die off and all the young ones will be (Eucalyptus patients) unless we do something different.”
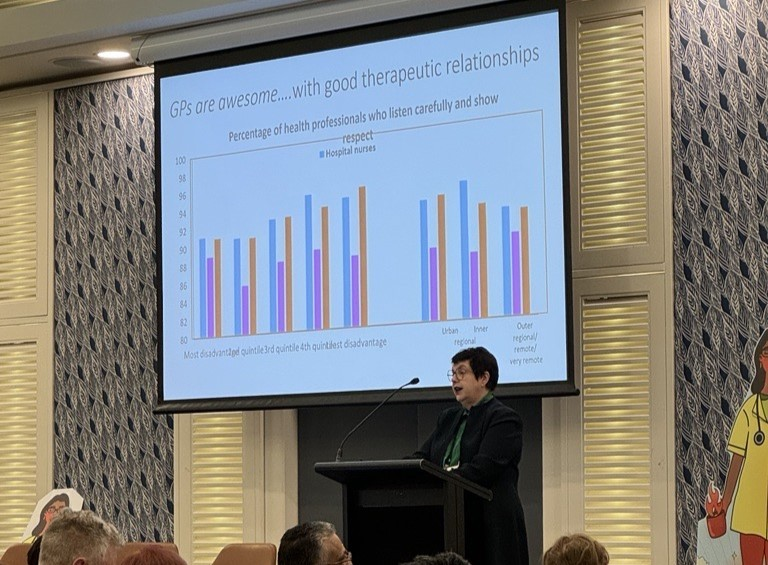
6. The numbers speak for themselves
The Australian National University Associate Professor (and GP) Louise Stone highlighted a 42% pay gap between men and women GPs. She said this was compounded by women GPs shouldering a majority of longer, underfunded consultations with complex patients, (who may have been released from hospital prematurely to reduce bed blockages).
7. But metrics may deceive
Associate Professor Stone cautioned that ‘evidence-based solutions’ in healthcare may not be what they seem. Analysis had shown the typical participant in clinical trials is a privileged white male, the researcher is likely to be a white urban male and even the average lab rat is a white furred male. This means clinical metrics may not be representative … and AI tools risk exaggerating biased data even further.
Evrima Technologies CEO and Founder Charlotte Bradshaw said that 80% of clinical trials are delayed in Australia because eligible people can’t be found and paired with researchers.
8. The My Health Record (MHR) will grow exponentially
Mr McCabe confirmed legislation is imminent to mandate sharing diagnostic imaging and pathology with the MHR. The government will also “push very hard” for every medication event – prescribing and dispensing – to be uploaded. The CSIRO-led Sparked community will need to lead the software industry to a FHIR (Fast Healthcare Interoperability Resources) standard to achieve this. Mr McCabe said Australian healthcare was hamstrung by “a lot of technology built in the 1990s that is not fit for purpose”. The recent MediSecure data breach showed, “We need to make sure we set the bar a lot higher than it is today”.
9. Technology knowledge is variable
When you’re a time poor GP, technology is rarely top of mind. You just want it to work. GPs still need reassurance from healthcare influencers that cloud technology is as safe (or safer) than server-driven desktop tech and that switching brings cost and time savings on hardware, hosting, back-ups, security, software patches, electricity and more. As one GP said to us, “You mean I can sack my IT guy?”
As for innovations such as Artificial Intelligence (AI), there’s a sense that while there are time, safety, revenue and efficiency gains to be made, the early adopters and innovators will be waiting a while for their conservative colleagues to join them.
10. Summing up
Based on our conversations and observations at Burning GP, community general practitioners feel underfunded, overworked, undervalued, and under siege from telehealth providers and pharmacists. They’re a resilient mob though, and still passionately defending their role as number one for longitudinal patient care.

*MediRecords new Admissions module means we can provide a longitudinal record connecting primary and tertiary care in one secure, cloud-hosted software system. We can send Discharge Summaries from our Admissions module and store them against the central patient file. Please reach out to us at sales@medirecords.com if you’re trying to solve these types of connectivity problems!