October 22, 2024
AI tools: What GPs think

Most GPs believe innovation improves patient health outcomes, yet only eight per cent of them identify as innovators and 35 per cent as early adopters, a new report has found.
The RACGP’s Health of the Nation 2024 report revealed that while the majority of GPs regularly use digital technologies — such as electronic prescribing — only 13% felt well-informed about innovations within general practice.
The report, in its eighth year, surveyed 3006 practising GPs.
This year, GPs were asked about their perceptions, attitudes, and behaviours regarding innovation in general practice, including:
- adopting new care delivery methods, such as telehealth;
- improved communication between healthcare professionals, including interoperable health records; and,
- new mechanisms to enhance patient care, such as patient enrolment schemes like MyMedicare.
GPs identified funding incentives as the most significant enabler of innovation in general practice, with 60% highlighting this factor.
While one survey respondent enthused, “Innovation has significantly enhanced general practice, particularly through technology”, 83% of GPs reported that they rarely or never use artificial intelligence tools.
GPs were asked, ”What new innovative practices or methods do you believe should be adopted to positively impact the care you provide?” They said:
- electronic health records, which improve care coordination and reduce errors
- telemedicine, which increases accessibility
- AI-driven tools
- systems that talk to each other/improved interoperability
- streamlined administrative systems that analyse business data
- new models of care
- multidisciplinary care
- a health status dashboard for patients to see what is recommended for their age
- remote monitoring, including wearable devices and health apps that empower patients to monitor their health
“Overall, these advancements save time, enhance accuracy, and enable more personalised healthcare, ultimately improving patient outcomes and the efficiency of general practice,” a GP summarised.
Regarding using AI scribe tools, one GP expressed increased job satisfaction after adopting the technology: “A happy GP is a good GP, and I’m even reconsidering my retirement plans.”
Founder and CEO of MediRecords Matthew Galetto commented that the report’s chapter on innovation “notably omits discussion of cloud and related technologies as a key enabler of digital innovation in primary care practices”.
“The report also lacks mention of the government’s initiative to promote real-time information sharing using FHIR (Fast Healthcare Interoperability Resources) standards, which are essential for interoperability and seamless patient care,” Mr Galetto said.
“FHIR is also a key enabler of digital innovation.”
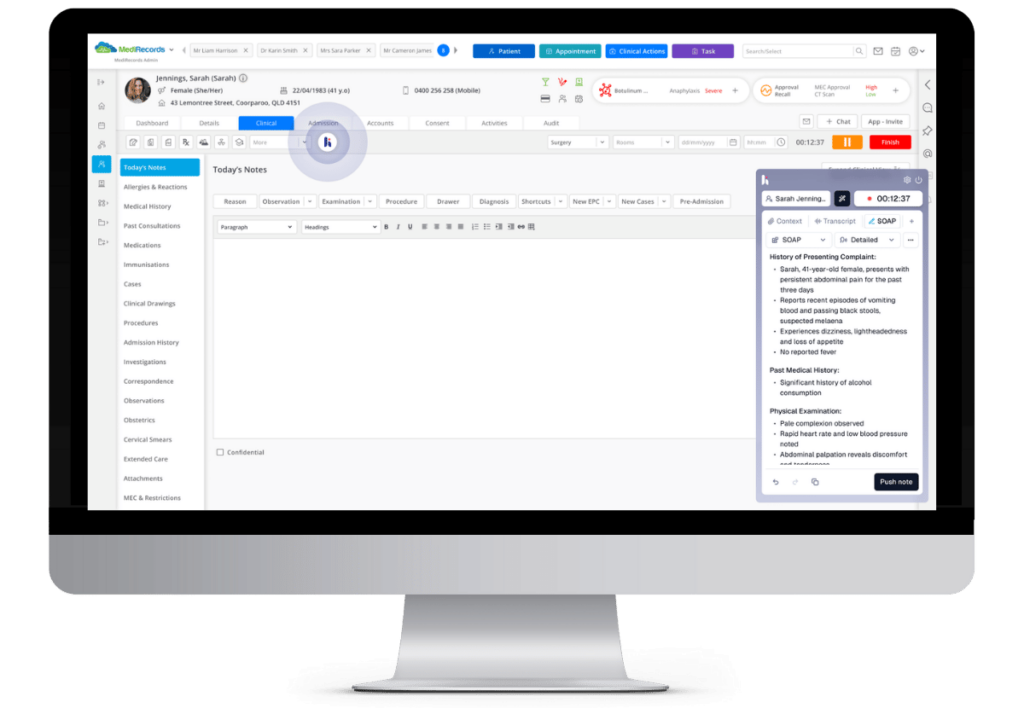
MediRecords is a leading digital innovator in healthcare, delivering cloud-based solutions built to FHIR standards across a diverse range of medical environments, from primary to tertiary care. Its recent integration of Heidi AI Scribe, an advanced AI tool powered by Heidi Health that streamlines clinical documentation, reinforces MediRecords’ commitment to digital innovation. Learn more about the partnership between Heidi Health and MediRecords here.