June 13, 2024
Solve Healthcare Challenges with MediRecords APIs

Effective management and secure sharing of clinical data are essential ingredients for providing safe, high-quality patient care.
However, healthcare providers often encounter challenges, from incompatible software systems to co-ordination issues among healthcare teams. In an effort to break down these barriers, MediRecords has developed a comprehensive suite of APIs to streamline data sharing processes and help improve patient outcomes.
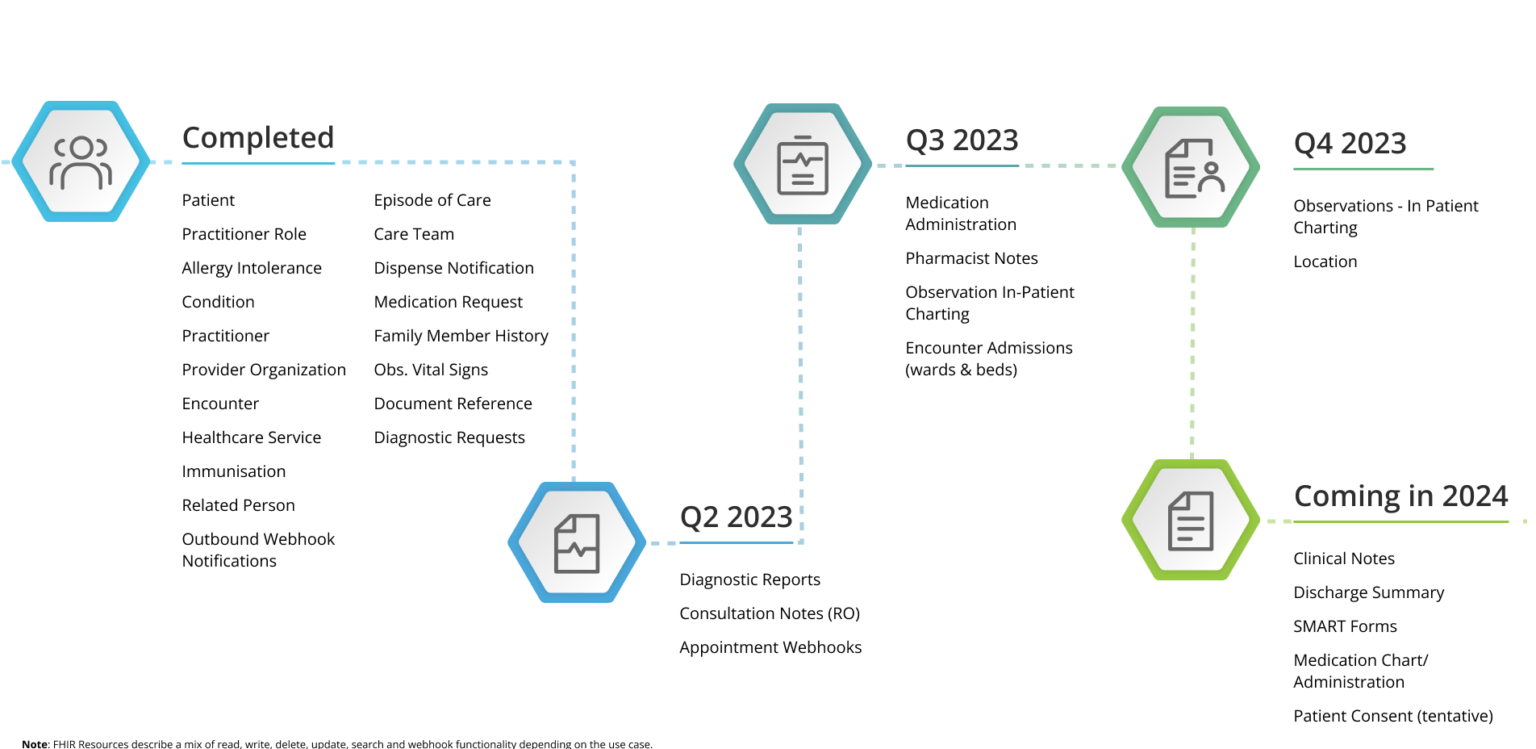
FHIR APIs: Elevating data management in healthcare
MediRecords’ FHIR APIs give you better access to and control of your clients’ clinical data by facilitating the management and sharing of patient records. From encounters to prescriptions, allergies to immunisations, these APIs offer a robust way to handle diverse sets of patient information. By enabling interoperability between systems, FHIR APIs ensure that critical data is accessible whenever and wherever it’s needed.
Connect APIs: Seamless integration for enhanced patient care
Complementing our FHIR APIs, MediRecords’ Connect suite of proprietary REST APIs offers a tailored solution for managing patient administrative data and other crucial information. From appointments to practitioner sessions, these APIs facilitate seamless communication and coordination among healthcare providers, resulting in more efficient care delivery.
FHIR & MediRecords APIs
FHIR is the future standard for health data interoperability. MediRecords has enabled FHIR as a mechanism for secure data exchange, including with hospital systems.
MediRecords has various APIs, including:
Patient
Securely exchange patient data with 3rd party systems, import patient records or notes into your database, create surveys and web forms to update the patient database, and update patient files from remote hardware devices or services.
Appointments
Our platform offers medical integration & scheduling with 3rd party booking systems & the ability to sync multiple clinicians' calendars to improve patient flows. We also provide reporting software integration for recurrence & patient 'no-shows'.
Correspondence
Easily filter & arrange correspondence in MediRecords and third-party applications. Initiate reporting, create actions or follow-ups, and use webhooks to push correspondence triggers.
Configuration
Utilise 'custom fields' in patient records to introduce additional patient identifiers. You can also create, update, and delete tags to categorise patient records and improve searching and filtering.
Key challenges MediRecords can address through APIs
- Integrated appointment booking: You can eliminate scheduling conflicts and incomplete calendars by enabling patient booking and appointment management across systems. For example, external booking software can be used to populate your MediRecords appointments calendar.
- Secure communication of clinical information: Ensure effective and safe communication of clinical information through secure sharing of patient material, including referrals and medical certificates, with data clinically coded to SNOMED standards, aligning with industry best practices.
- Unified patient identifier: Overcome the challenge of duplicate patient records by sharing a unique patient identifier across systems, thus ensuring synchronized and accurate patient information. This identifier becomes the key to making sure systems and data are in synch.
- Consolidated patient record data: Provide a consolidated view of extended patient details by integrating patient demographics, allergies, conditions, and family history across systems. For example, if a patient’s details are updated in MediRecords, you can use APIs and webhooks to make sure these same details are updated in a separate client management system (CMS).
- Closed-loop medication ordering: Enhance medication management by monitoring orders from prescription to dispensing, thereby minimising errors and disruptions in patient treatment plans. An example is the sending of evidence of prescription from MediRecords into a hospital enterprise system, creating a single source of truth for medication history. MediRecords has done this at Northern Health in Melbourne, to support Victorian Virtual Emergency Department prescribing workflows.
- Integrated case management and shared care: Improve collaboration among healthcare teams by integrating episode of care details, ensuring a more coordinated approach to patient management. Updating the status of allergies and investigation requests, for example, can increase safety and reduce risk of duplicated procedures.
- Flexible data capture and retrieval: Offering flexibility in capturing and retrieving custom data through custom fields within MediRecords, tailored to specific practice needs.
Learn more about the problems MediRecords APIs can solve here.
MediRecords’ APIs represent a significant step forward in addressing the complex challenges faced by healthcare providers today. By offering robust solutions for data management, communication, and collaboration, these APIs empower healthcare teams to deliver safer patient care in an increasingly interconnected healthcare landscape. With a commitment to innovation and efficiency, MediRecords will continue to expand our means of securely sharing the data needed for the future of healthcare delivery.