September 20, 2024
Aussies’ Sexual Health Trends: Insights for Sexual Health Month
Sexual Health Month provides a timely opportunity to survey some of the recent research in the field of sexual and reproductive health — and report some news from the coalface.
Travellers
Travelling Aussies are mostly proactive about their sexual health before departure when they see a travel-medicine doctor or nurse, with 72% of those in the study requesting STI testing pre-departure.
Over 60s
A survey of 1840 people aged over 60 found patients want GPs to initiate sexual health conversations as part of routine care. It also found that barriers included patient embarrassment, uncertainty about finding solutions, and ageism.
James Sneddon, co-founder of Stigma Health, said that while the largest age group accessing STI testing via his service is 20-30, the next biggest bracket is those aged 60-70, “with an influx of those who are pushing 80”.
Prostate cancer
Information on complications with sexual function following prostate surgery are the most commonly unmet need among men with prostate cancer, a study found. The researchers recommended sexual well-being discussions as standard care for all prostate cancer patients.
Women’s health
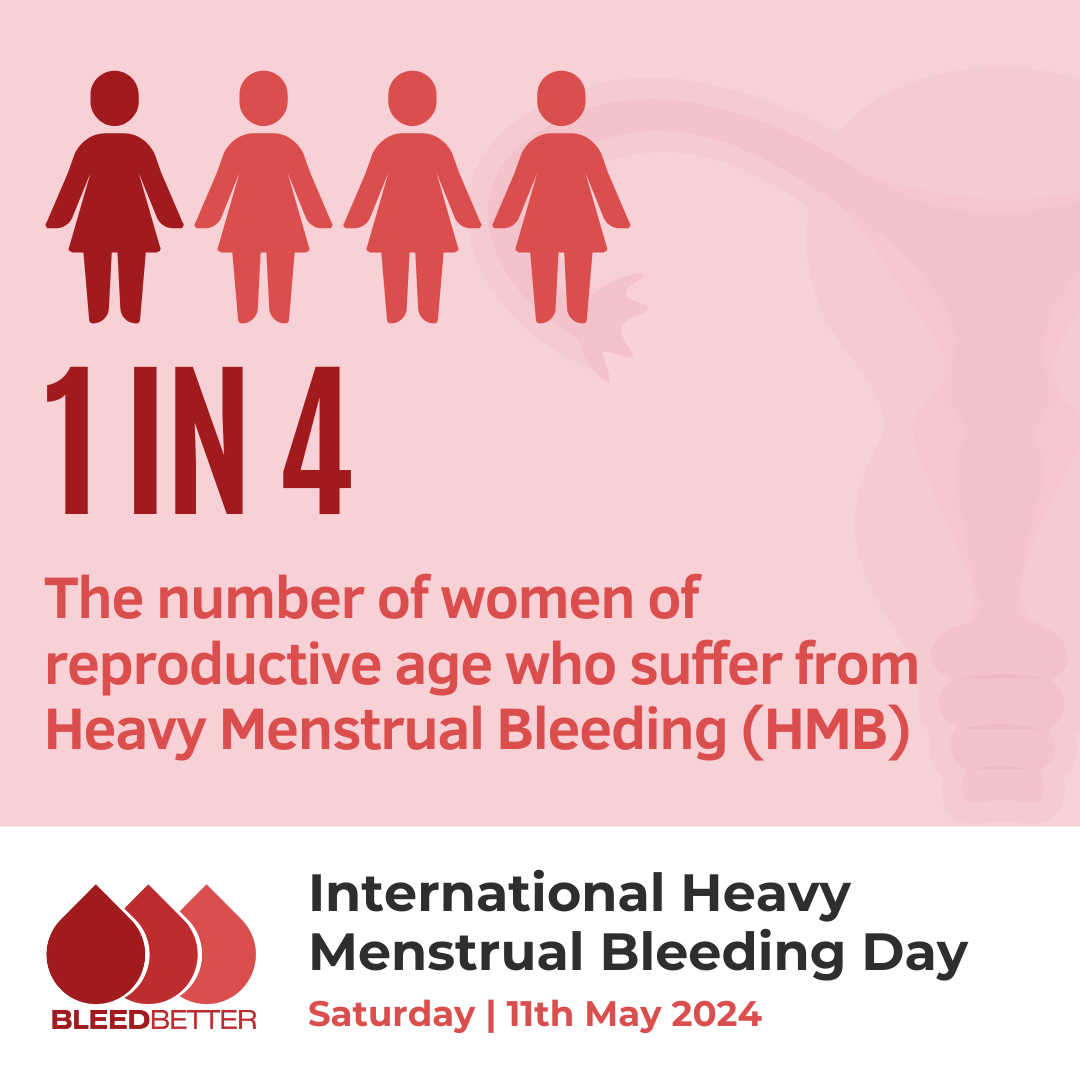
A special edition of the Australian Journal of Primary Health dedicated to optimising women’s sexual and reproductive health in primary care highlighted that:
- There is a high level of unmet need for effective contraception in Australia and access barriers including the availability of services.
- The limited number of GPs who insert intrauterine devices presents a significant barrier to access.
- Access to abortion care in Australia is inequitable, especially outside cities, and few publicly-funded abortion options are available in most states.
- There is an urgent need for transparency around public abortion service availability and government commitment to expanding abortion care.
- Most women did not receive in-depth contraceptive counselling antenatally or postnatally, but would have found this useful.
- Women surveyed about over-the-counter access to the oral contraceptive pill were in favour, especially for repeat prescriptions.
Awkward
For sexual health month, the key message from Mr Sneddon is: “Get awkward. Have a conversation with your mates or your partner about getting tested; the majority of STIs have no symptoms.” Among Aussies tested via Stigma Health, there has been a recent surge in Chlamydia numbers; it is 33% higher than the 5-year mean, Mr Sneddon said.
Further reading:
Ahmed, Z., Gu, Y., Sinha, K., Mutowo, M., Gauld, N., & Parkinson, B. (2024). A qualitative exploration of the over-the-counter availability of oral contraceptive pills in Australia. PloS one, 19(6), e0305085.
Bourchier, L., Temple-Smith, M., Hocking, J. S., & Malta, S. (2024). Older patients want to talk about sexual health in Australian primary care. Australian Journal of Primary Health, 30(4).
Charlick, M., Tiruye, T., Ettridge, K., O’Callaghan, M., Sara, S., Jay, A., & Beckmann, K. (2024). Prostate Cancer Related Sexual Dysfunction and Barriers to Help Seeking: A Scoping Review. Psycho‐Oncology, 33(8), e9303.
Dev, T., Buckingham, P., & Mazza, D. (2023). Women’s perspectives of direct pharmacy access to oral contraception. Australian Journal of Primary Health.
Haas, M., Church, J., Street, D. J., Bateson, D., & Mazza, D. (2023). How can we encourage the provision of early medical abortion in primary care? Results of a best-worst scaling survey. Australian Journal of Primary Health, 29(3), 252–259
Li, C. K., Botfield, J., Amos, N., Mazza, D. (2023) Women’s experiences of, and preferences for, postpartum contraception counselling. Australian Journal of Primary Health 29(3), 229-234.
Mazza, D., & Botfield, J. R. (2023). The role of primary care in optimising women’s sexual and reproductive health. Australian Journal of Primary Health, 29(i–iii).
Power, A., Tuteja, A., Mascarenhas, L., & Temple-Smith, M. (2023). A qualitative exploration of obtaining informed consent in medical consultations with Burma-born women. Australian Journal of Primary Health, 29(3), 284–291.
Srinivasan, S., Botfield, J. R., & Mazza, D. (2023). Utilising Health Pathways to understand the availability of public abortion in Australia. Australian Journal of Primary Health, 29(3), 260–267
Warzywoda, S., Fowler, J. A., Debattista, J., Mills, D. J., Furuya-Kanamori, L., Durham, J., … & Dean, J. A. (2024). The provision of sexual and reproductive health information and services to travellers: an exploratory survey of Australian travel medicine clinicians. Sexual Health, 21(1).
Stigma Health eliminates embarrassment by removing the need for in-person clinical consultations and allowing consumers to get a non-confrontational STI-test pathology referral online then take it to any of the 10,000 pathology collection centres Australia-wide.