September 21, 2021
How MediRecords has taken remoteness away from general practice.

Andrew Dyson, Digital Health Business Consultant
NetMD are a medical centre with a difference. Their aim is to use modern technology to deliver general practice.
NetMD do this, using MediRecords, Coviu and e-scripts, to offer medical teleconsultations online. Sixty percent of their consultations are now performed this way.
The Challenge
“I was working with Medical Director,” says NetMD general practitioner, Dr Leo Gunaseelan, “It cost $80 to $100K to install, plus a technician to fly from Cairns to do this at $3K a day, and yearly maintenance costs of $15 to $20K. With MediRecords I can manage everything myself, and I don’t need anyone’s help. I have freedom.”
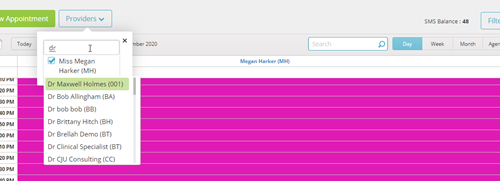
Dr Gunaseelan specialises in family medicine and rural medical care. He runs NetMD as an online teleconsulting service to ensure he is accessible to patients, no matter where they are based.
“I have been working with MediRecords for five years,” says Dr Gunaseelan, “They are great, and have good support staff. MediRecords are fully cloud-based and I never need to take a day off. I have one week away a month and just work from wherever I am. That way, my patients don’t miss out on treatment.”
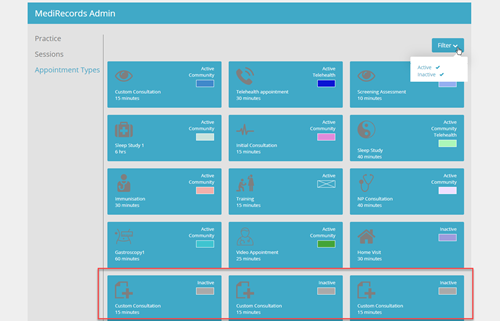
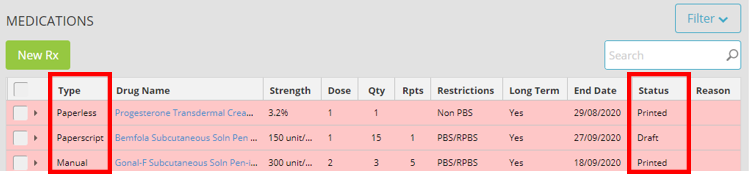
How is MediRecords Used?
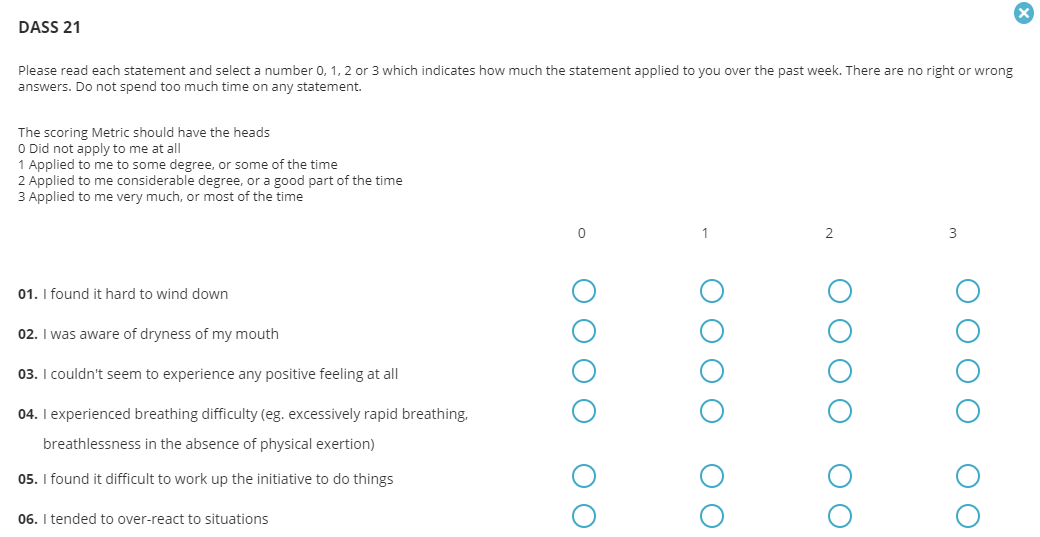
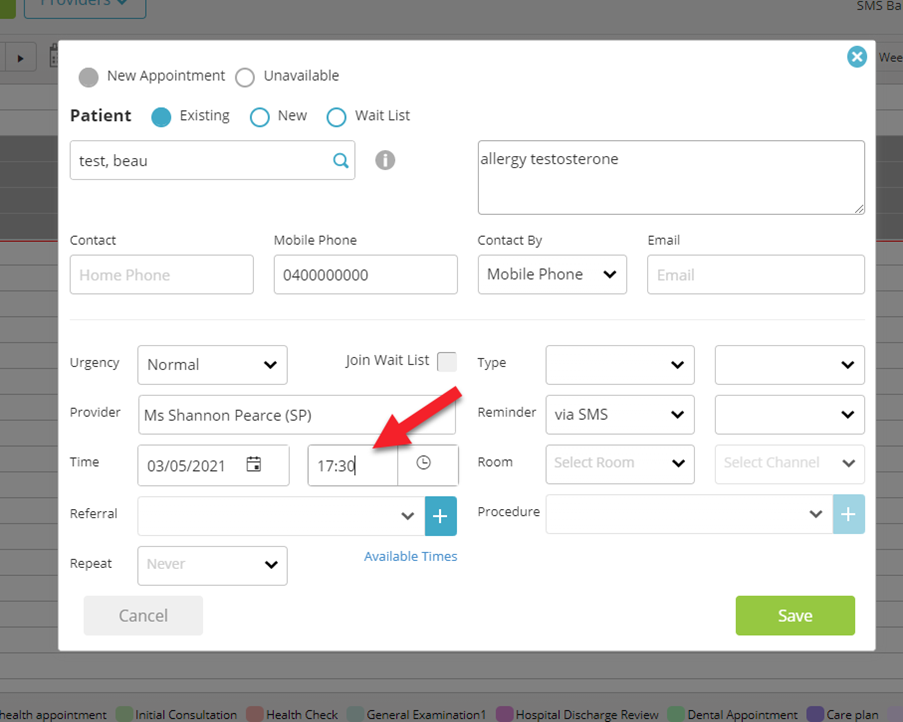
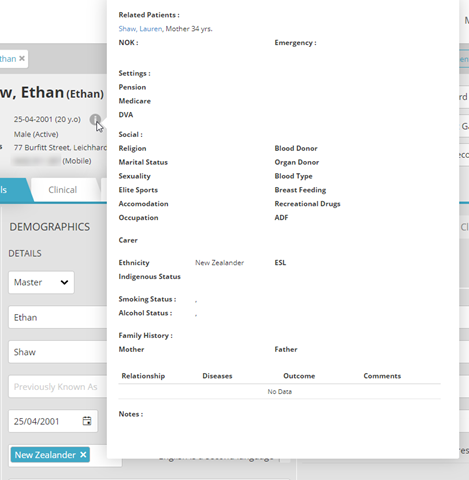
Patients don’t need any special equipment to access NetMD services– just a phone, and a mobile or internet signal.
“Patients love it,” says Dr Gunaseelan, “You don’t need high quality internet- just a satellite signal will do. Patients don’t need to come into the practice. I can provide my services to them from anywhere in the world, and it’s working well.”
Dr Gunaseelan has been practicing for over 30 years, throughout rural New Zealand, Europe and the remote mining regions of Australia.
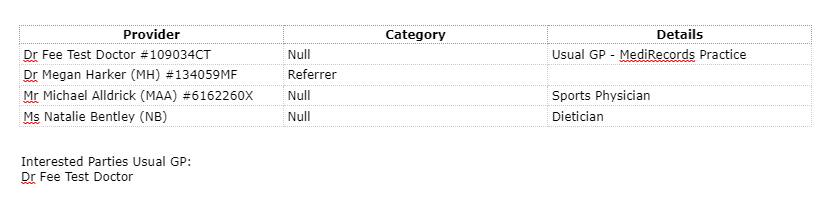
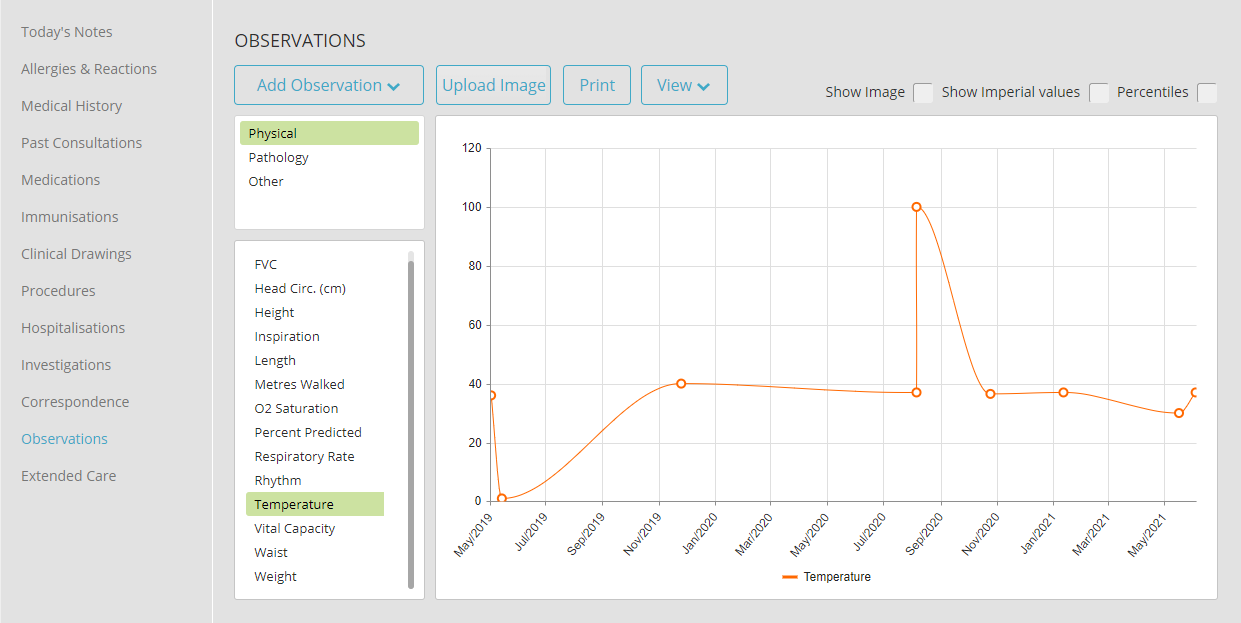
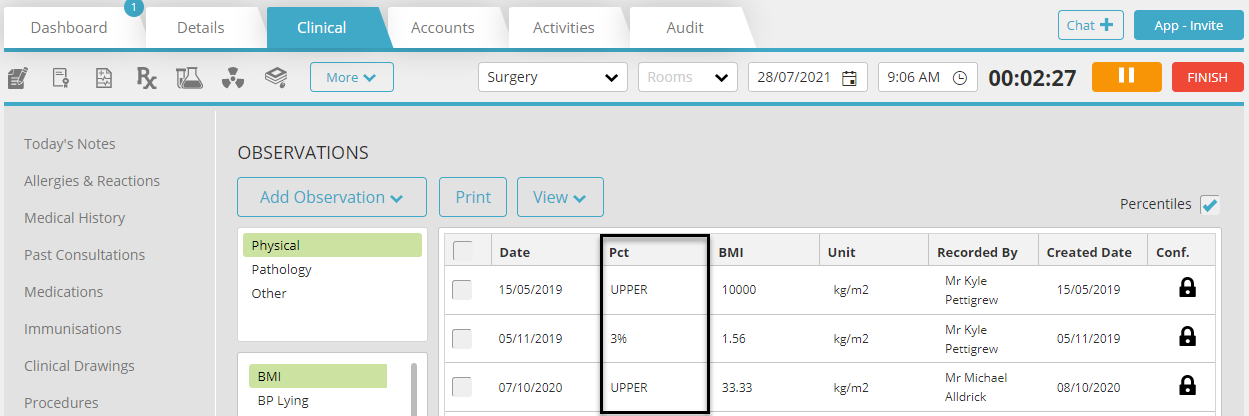
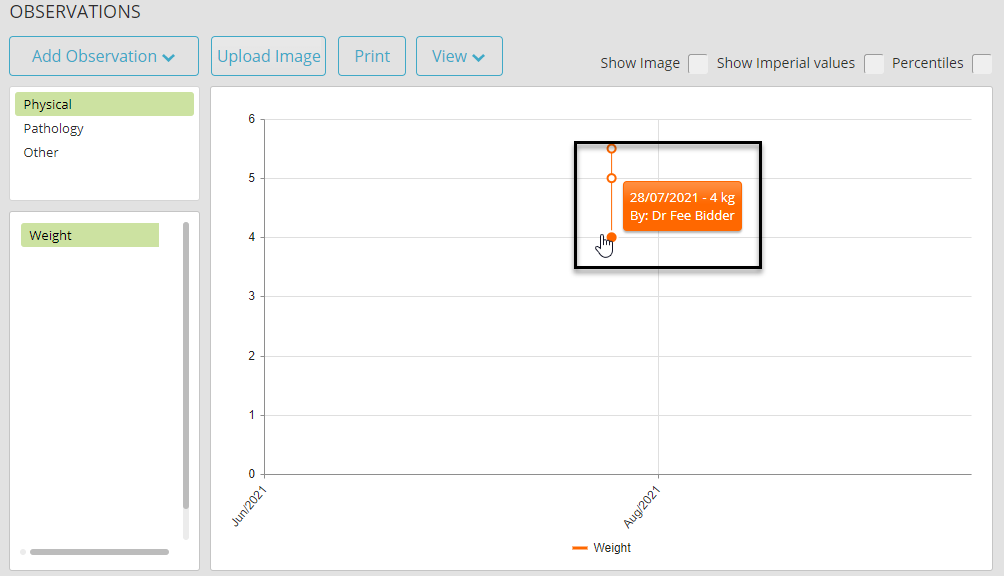
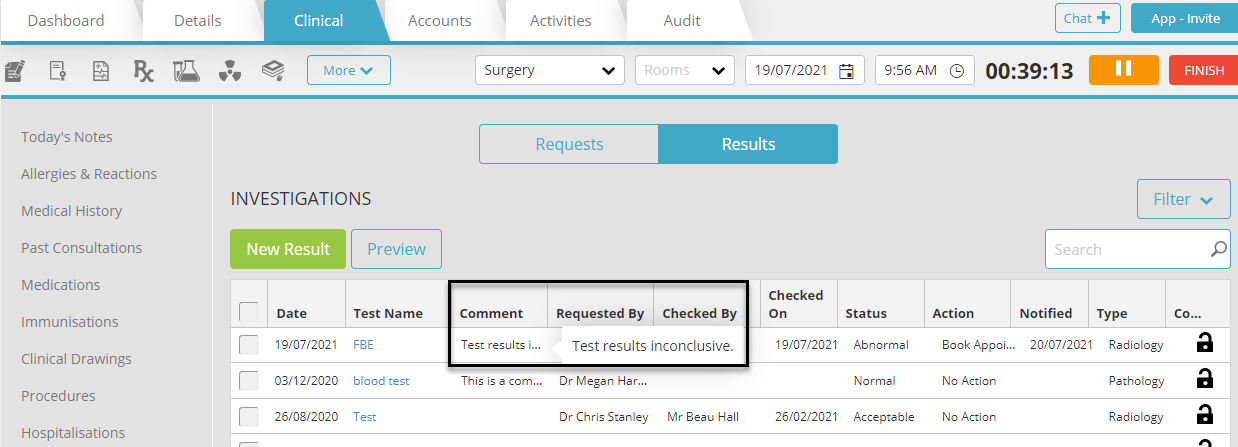
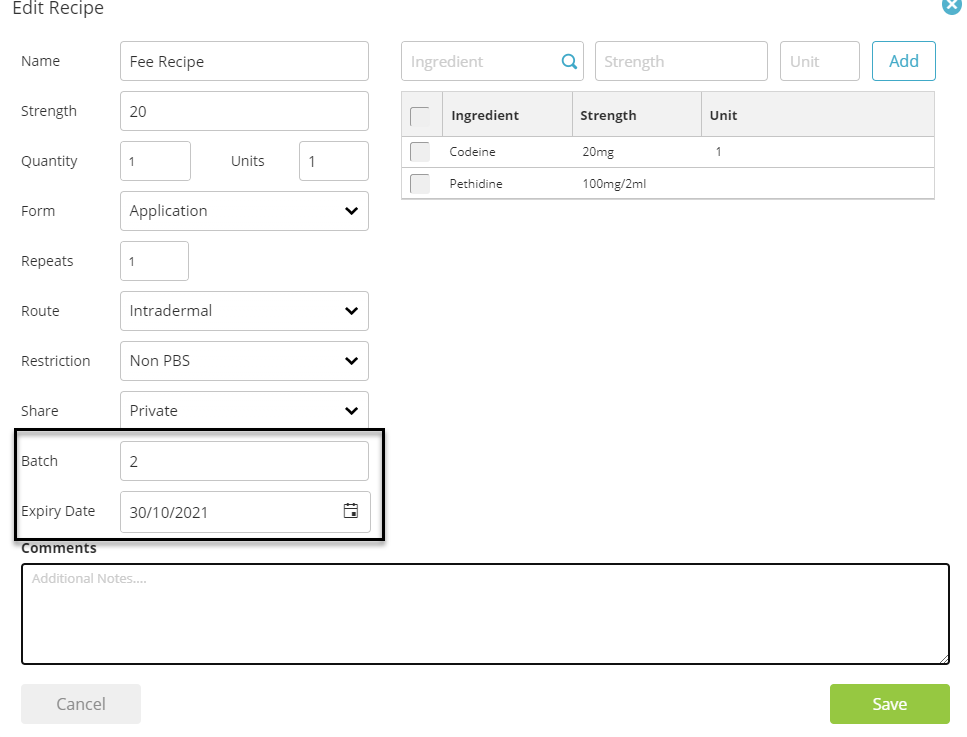
“My work with Rio Tinto involves looking after patients from Tasmania and remote Queensland. I can train medical staff in the mines to use and read the medical equipment, and then I can read the results from wherever I am. Remoteness has been taken away.”
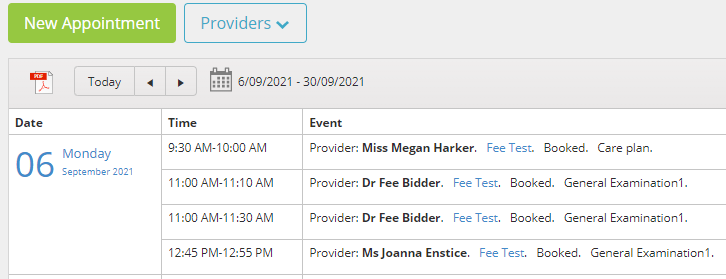
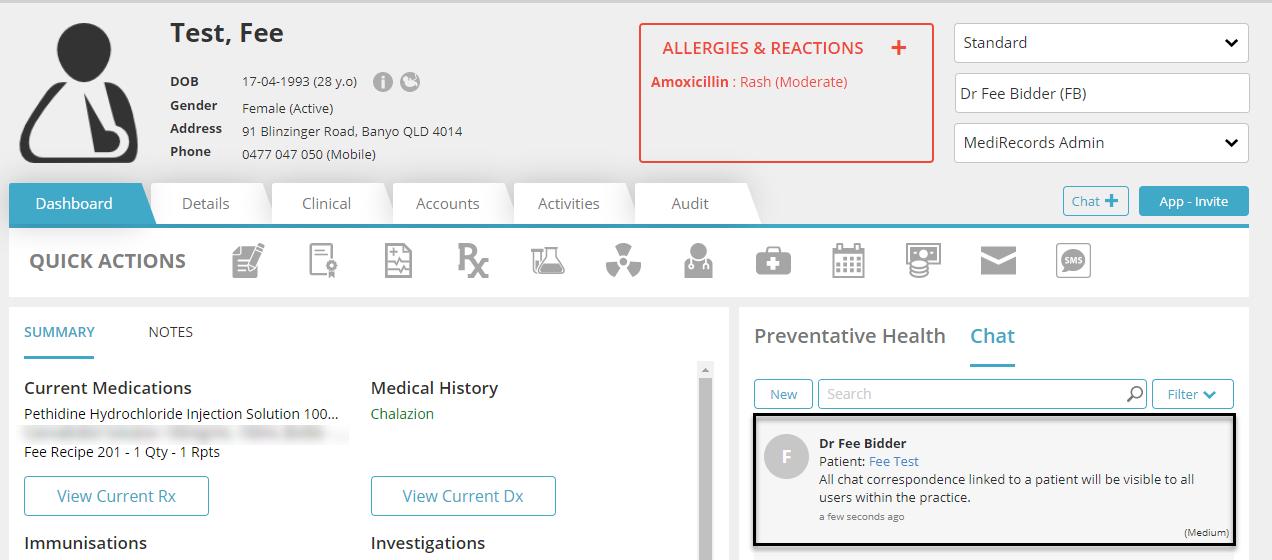
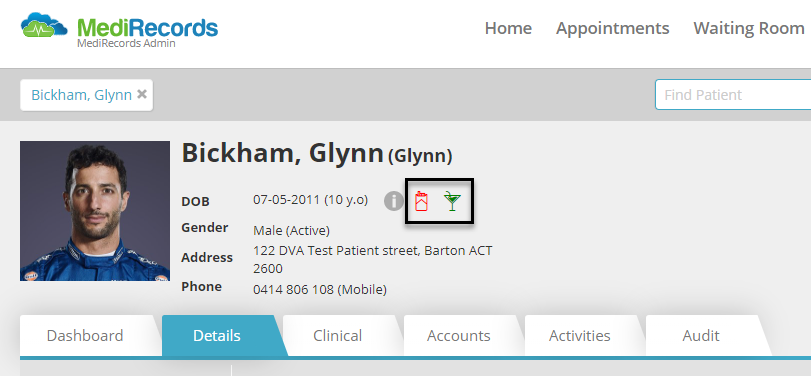
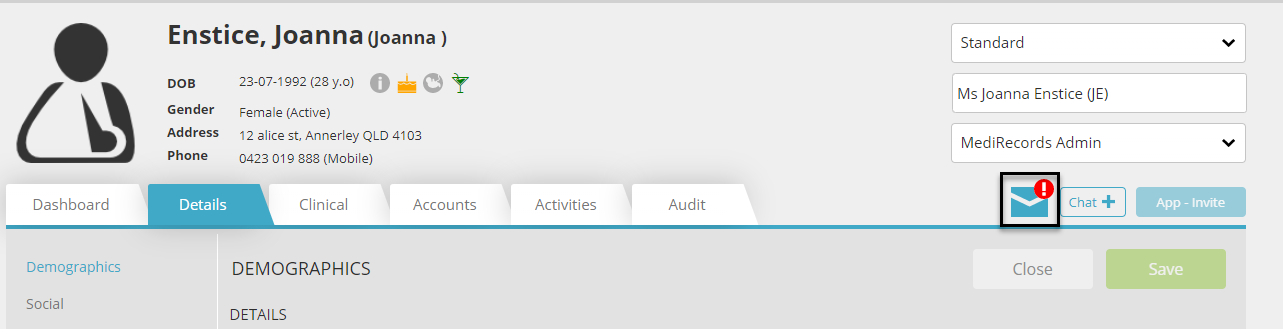
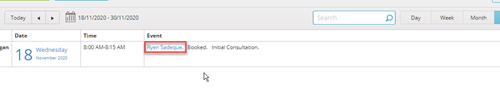
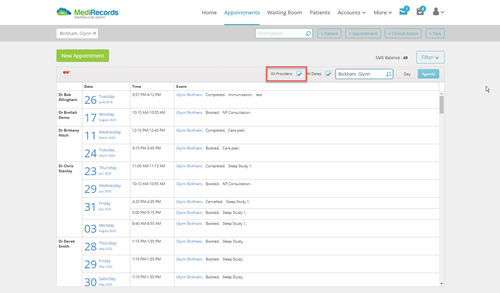
Patients can also book consultations on the NetMD website and use the MediRecords app to access test results straight away.
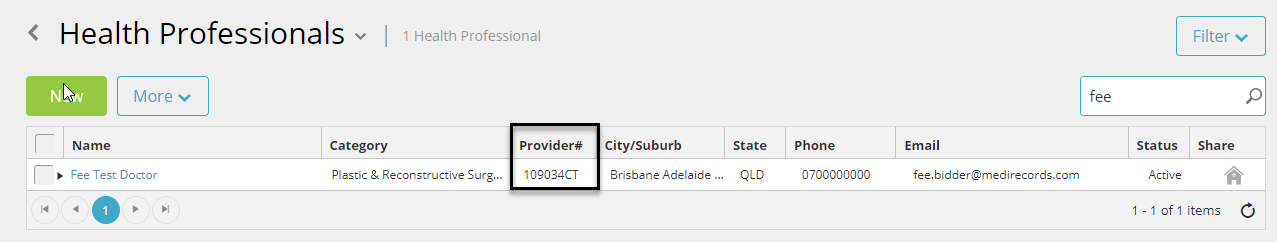
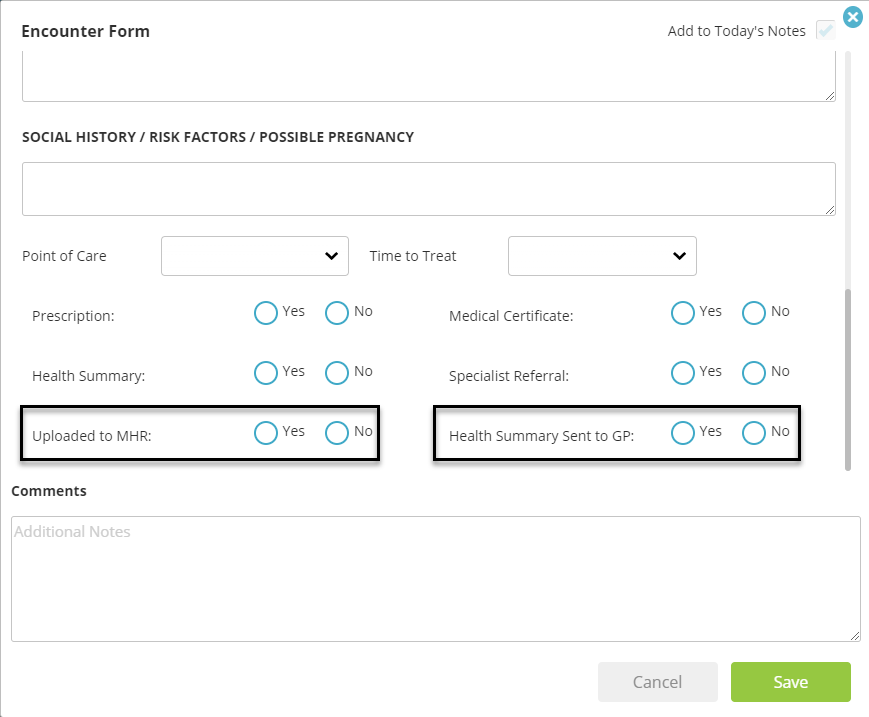
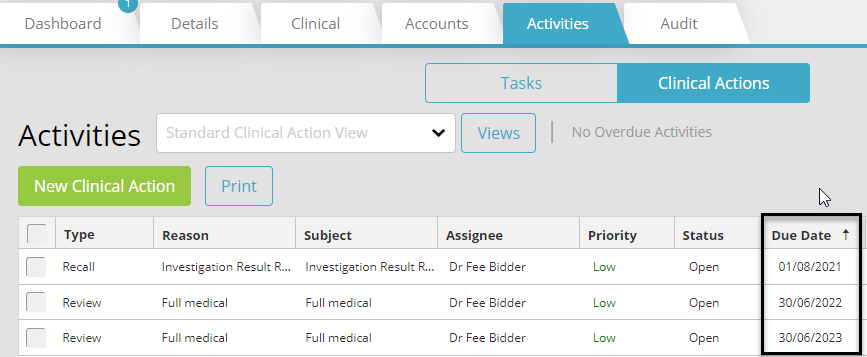
“The app is the main point of difference,” says Dr Gunaseelan, “I have 3,000 patients, and they all use it and check it regularly. Before, I had a nurse, who was only looking after recalls by phone and mail. Now I don’t need her- I just click a couple of buttons and a text is sent to my patient with a link to make an appointment. It’s as perfectly simple as that.”
In addition, MediRecords provides health to visitors to Dr Gunaseelan’s general practice.
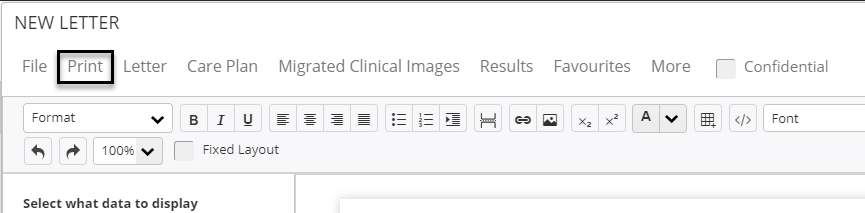
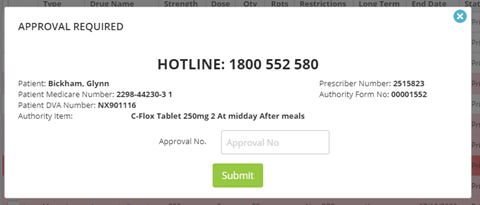
“I look after about 15,000 tourists every year,” says Dr Gunaseelan, “In two minutes they have the prescription they need emailed to their phone. They always say, ‘wow, why don’t we have this at home?’”
Looking Forward
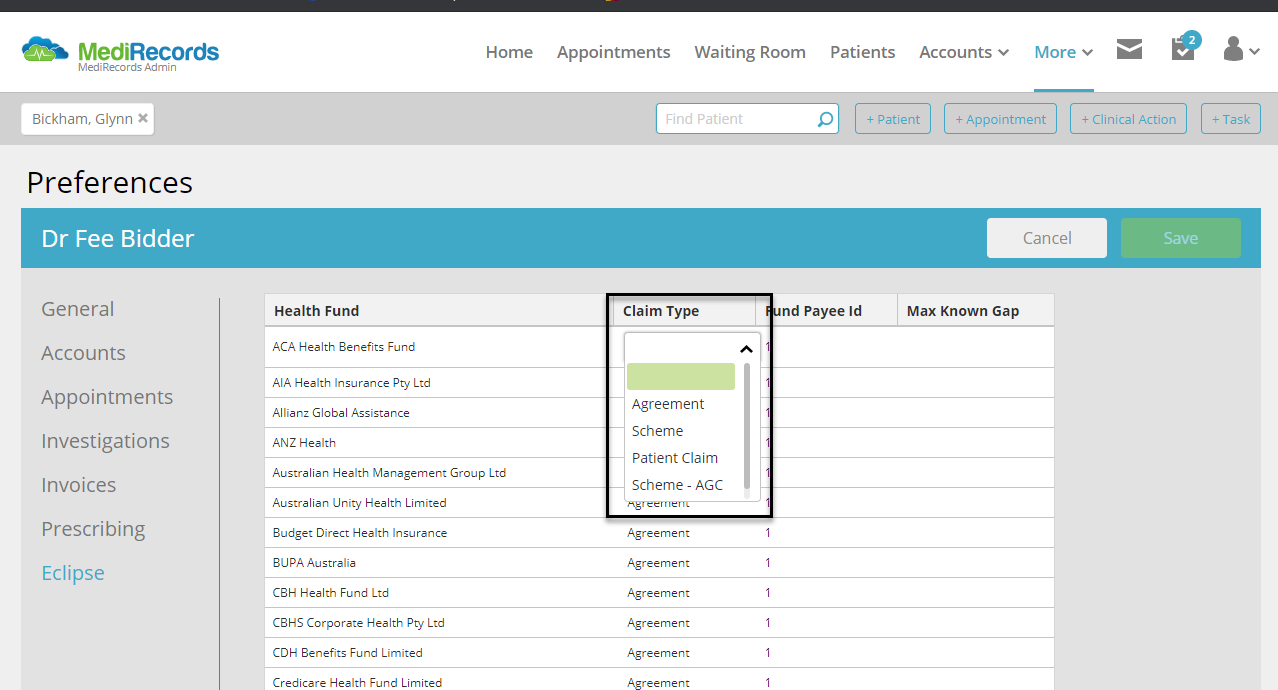
Dr Gunaseelan is so pleased with MediRecords that he plans to expand the reach of his services.
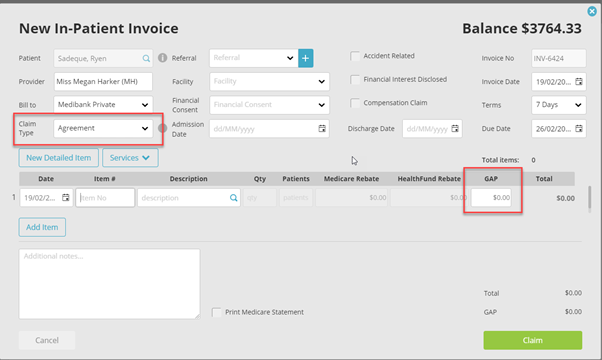
“I want to widen the breath of services we offer online, with payments being made available online, and I’m also working to integrate a YouTube channel by the end of next year,” says Dr Gunaseelan, “I want to extend my services to Papua New Guinea, the Solomon Islands and Samoa. I want to provide services for people that don’t have access. I have always wanted to do this, I just didn’t know how.”
“It’s a great program,” says Dr Gunaseelan, “If I could, I would promote MediRecords to anyone. They improve general practice immensely.”
For more information on NetMD and Dr Gunaseelan’s work visit netmd.com.au.
To find out how MediRecords can support your organisation to expand into virtual care and telehealth services, you can contact Michael Alldrick on email at michael@medirecords.com.