October 23, 2023
A clinician's MediRecords odyssey: unveiling efficient, mobile aged care medicine

Here’s the latest in our series on how people use MediRecords. In this Q & A, Dr Gaveen Jayarajan explains why he made the switch to the cloud and MediRecords to power his Doctors in Aged Care mobile medical practice.
Tell us a bit about your practice.
I operate the Doctors in Aged Care mobile GP service that visits residents at several Residential Aged Care Facilities (RACFs) throughout metropolitan Melbourne. Our service exclusively does RACF work and is fully mobile and virtual; we see residents in their homes every week. We are committed to excellence in medical care of the elderly using innovative, non-traditional/hybrid approaches to healthcare service delivery.
Associated with our medical practice, I have built the Doctors in Aged Care (DiAC) Facebook group, which is a community of over 2300 doctors Australia-wide.
Please contrast MediRecords with the system you used prior to using MediRecords.
I had used all the common GP clinical and practice management systems working as a GP in medical centres for the previous eight years. Usually clinics would use two different programs, one for clinical use and one for practice management (i.e., appointments/billing/claiming/reporting). When I started working full-time in aged care, I used a popular GP clinical software system which was server-based. This worked okay in a medical centre but was not well suited to mobile work visiting RACFs.
As a doctor working in a challenging and inefficient setting, I urgently needed a reliable and stable solution. Hence my move to a cloud-based alternative, MediRecords.
My initial apprehension with using a cloud system was what happens if internet speed and connection were unreliable? To my surprise this was a non-issue. Using mobile broadband devices, which now give NBN-type speeds in some locations, internet speed was not an issue. I could also use my mobile phone as a Hotspot if needed.
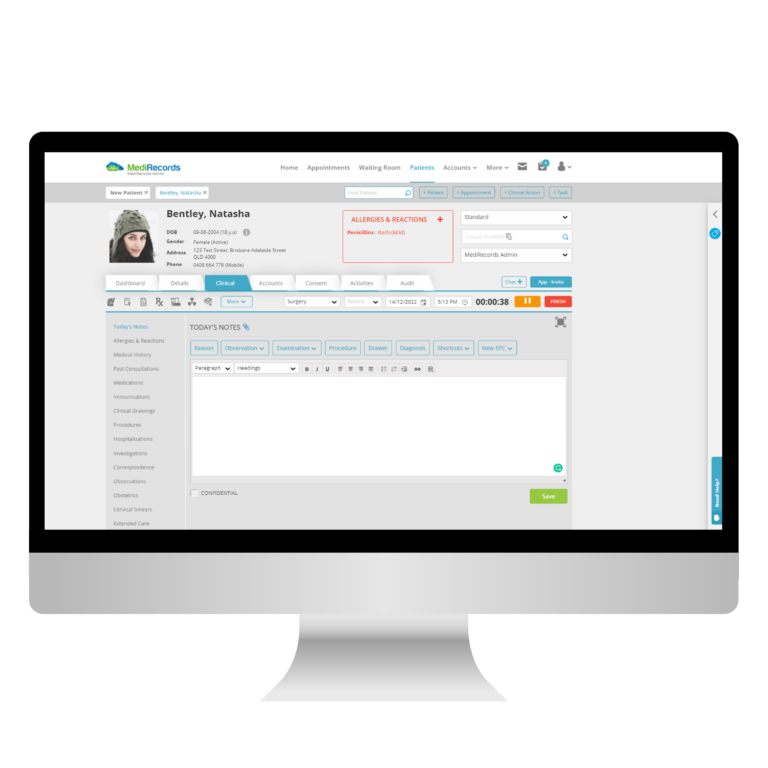
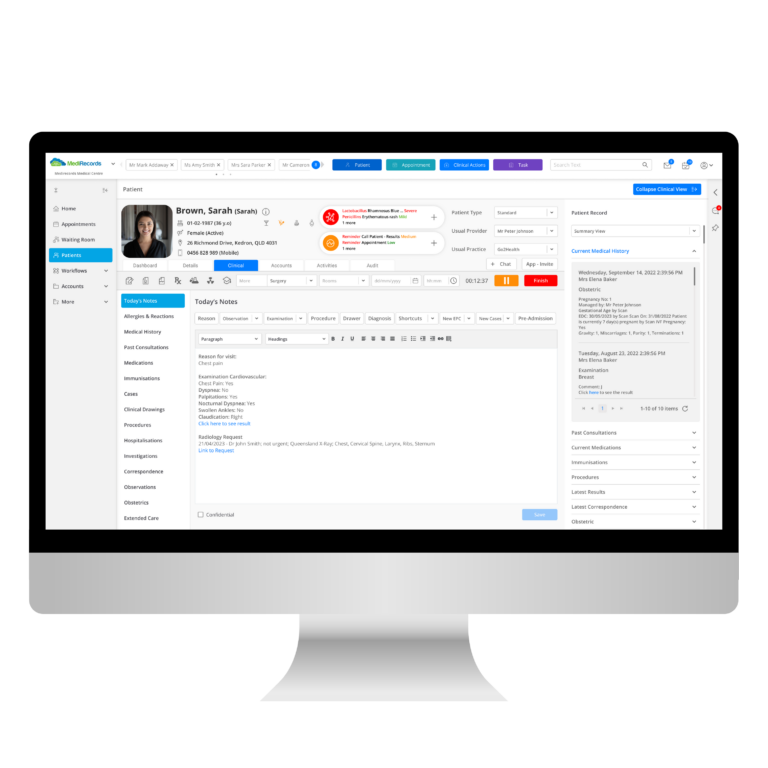
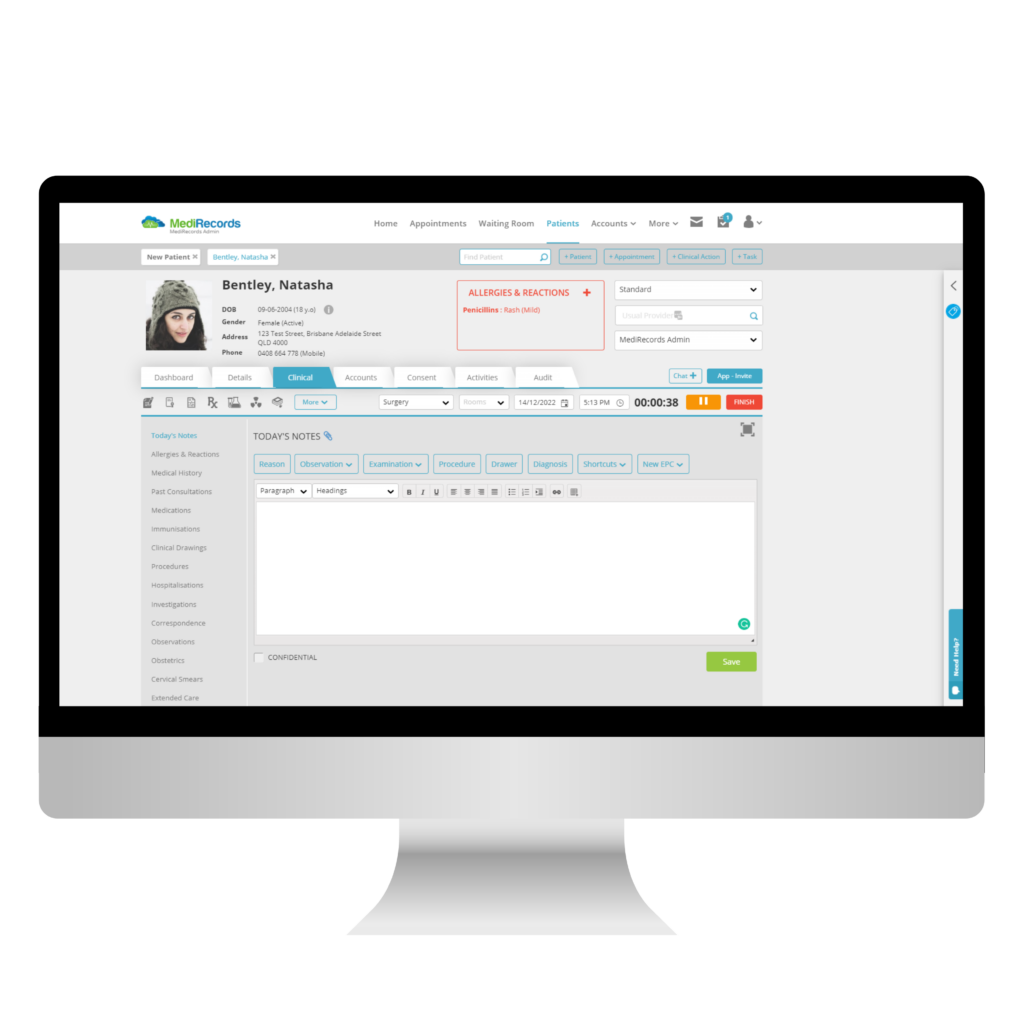
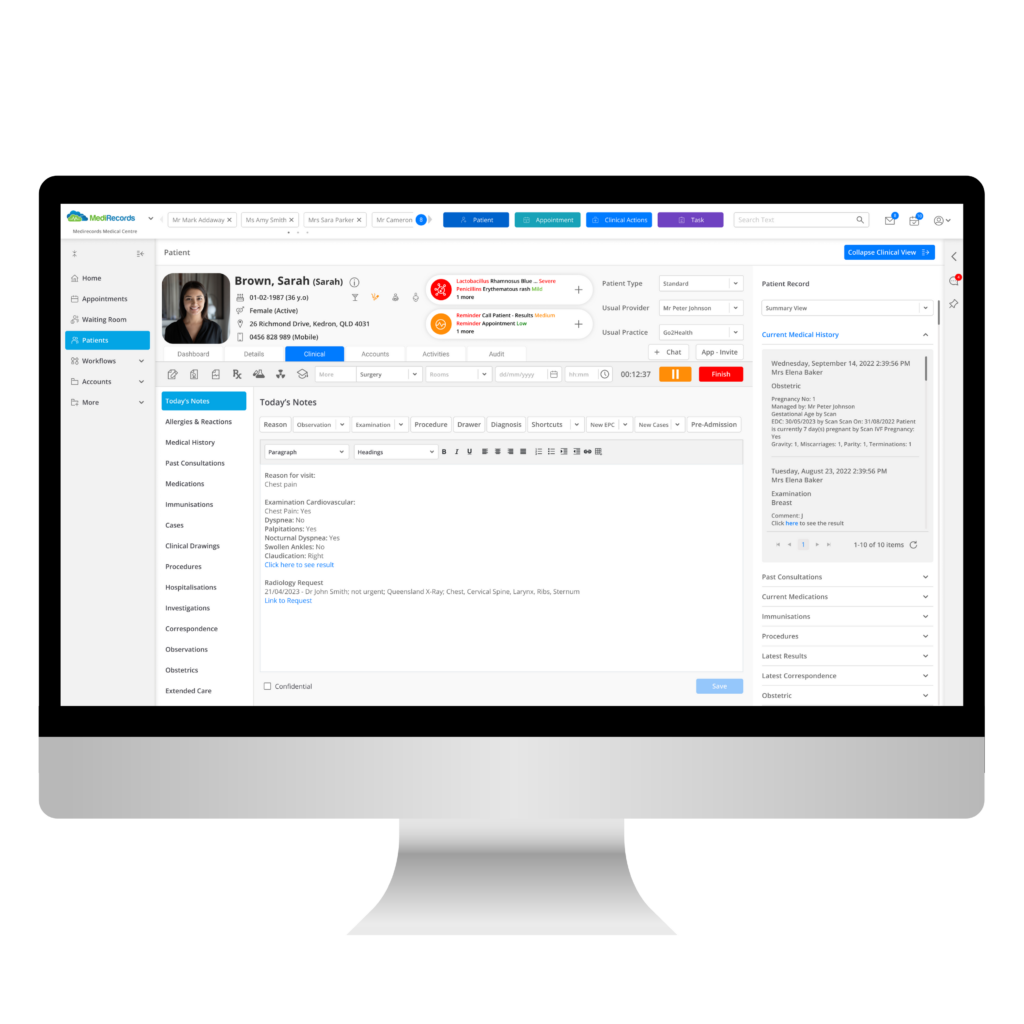
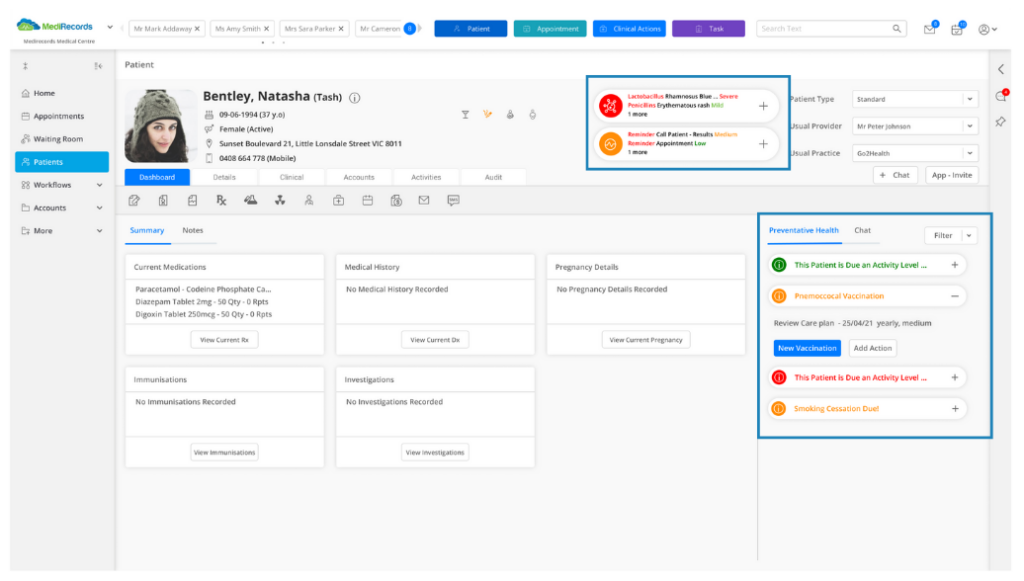
MediRecords is an all-in-one, integrated clinical and practice management system. So, from a single browser window I could access the clinical functions I needed as well as seamlessly view my appointment book, create new appointments, perform billings, view current Medicare claims in progress, and generate reports for total invoices/billings over any time period.
The third change was no longer having to engage and deal with a third-party IT service provider. Now all of this was handled in the background automatically; updates are installed remotely with no disruption or major technical issues.
How does MediRecords enhance your efficiency?
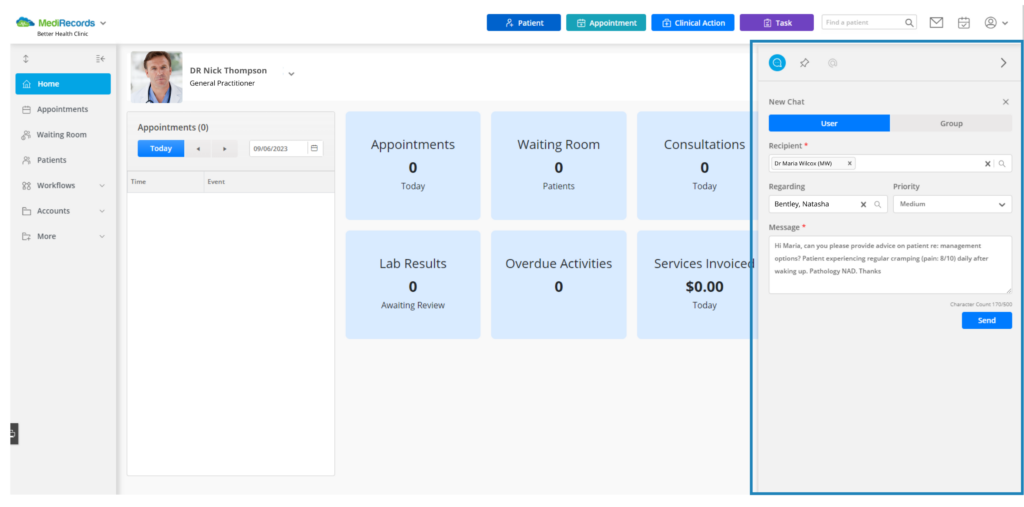
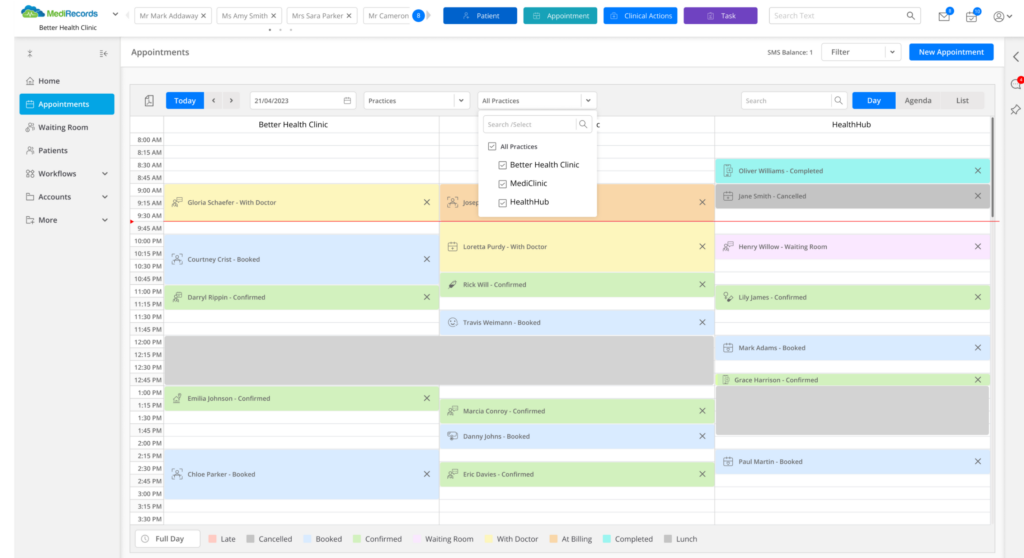
I use the MediRecords appointment book as a key tool to manage my workload, maximise efficiency and provide proactive rather than reactive care.
Every time a phone, email or fax request is received to review a patient, the patient’s name is entered into the appointment book for the next weekly visit day (or on the day of request if urgent) with an appointment type depending on the nature of the issue. It could be a “Regular” appointment or classified as for example, “Urgent’’, “Vaccine”, “Wound Review”, “Post-fall Review”, “Health Assessment”, “Phone Consultation”, etc. MediRecords allows multiple appointment types and durations to be created. Every time a patient is seen, a follow-up appointment is also made at an appropriate interval. When done for every patient, I can see with reasonable accuracy what my workload will be like. Unplanned extra patients, or “walk-ins”, can be added to the daily schedule depending on demand that day.
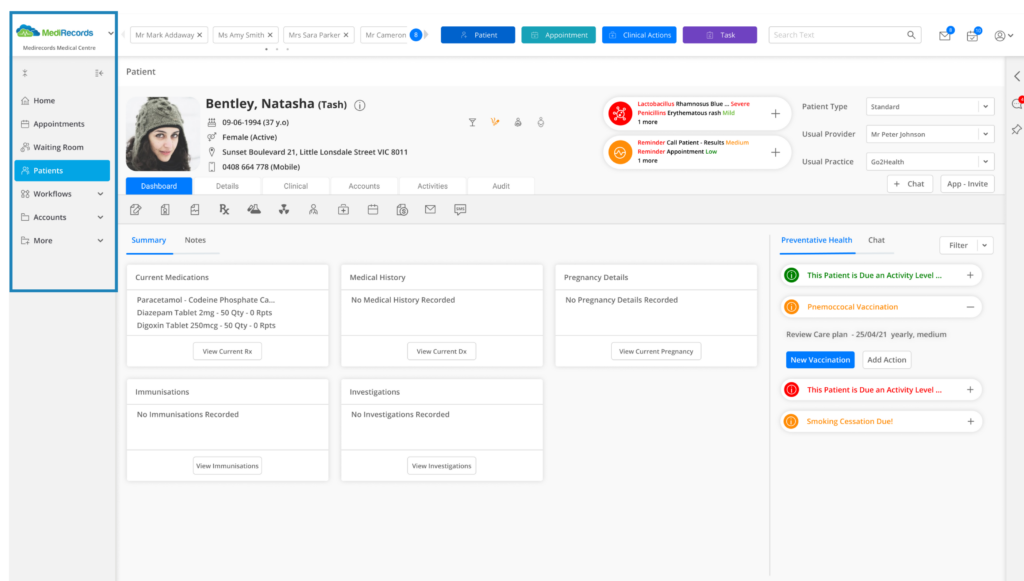
We further enhance our scheduled care by using the recalls or “Clinical Actions” function. For every new patient we have recalls for core things relating to Medicare item numbers and due dates, e.g., Health Assessments, Residential Medication Management Reviews and Care Plan Contributions.
Also useful for efficiency is the Tagging feature. I use Tags, along with another existing MediRecords feature of doing multiple patient invoices at once, to reduce the time taken to process daily billings to under five minutes.
Another recent improvement has come with my API integration of MediRecords with Snapforms. Using Snapforms I created a “New Patient Details Form”. Now when a RACF asks me to take on a new patient, I email them a cloud-based form with a URL link. They complete all new patient details, attach a recent patient health summary or hospital discharge summary and a current medication list. After they hit submit, something magical happens! A new patient file is created in MediRecords with the key demographic data already populated, and a PDF copy of the form and any uploaded health summary or discharge summary and medication lists stored in the Correspondence IN tab in the patient file.
I use MediRecords on multiple devices including my Surface Laptop, Samsung Galaxy tablet and Samsung Z-Fold 5 mobile phone.
How does MediRecords enhance patient care?
MediRecords allows me to operate with the lowest and leanest cost base and make it financially viable and sustainable for the long-term. It enables me to maintain safe and high standards of care that are consistent, repeatable and maximise quality of life for patients.
What are your tips for people considering changing to MediRecords?
Have a clear idea and rationale for why you want to move to the cloud.
It can’t just be about saving money on software subscription costs or on upgrading or buying a new server. Independent GPs working at your practice will not be interested in this. Show them a way forward with a big picture view of how moving to the cloud can change the way they deliver healthcare, creating benefits they are not currently experiencing. Avoid trying to replicate like-for-like every feature of server-based software.
What are you looking forward to with MediRecords in the future?
The efficiencies we have been able to achieve by using cloud-based software have been done with an intense focus on optimising processes and managing costs – and without Artificial Intelligence (AI). We look forward to incorporating AI to further drive efficiency and improve patient care standards by automating more administrative processes and providing advanced clinical decision support and insights.
If you’d like to showcase innovative ways you use MediRecords in healthcare, please reach out to us via sales@medirecords.com.
Dr Gaveen Jayarajan is an investor and member of the MediRecords Medical Advisory Board.
Read more about Doctors in Aged Care on their website.