August 8, 2023
It's a Yes from MediRecords for the Voice to Parliament


Tim Pegler - Senior Business Development Manager
MediRecords strongly encourages Australians to vote yes in the upcoming referendum for an Aboriginal Voice to Federal Parliament.
As a company committed to helping deliver better health outcomes for all Australians, MediRecords believes the Voice to Parliament is an essential step toward equity and justice for First Nations peoples and ‘closing the gap’ in indigenous health.
Closing the Gap
Aboriginal and Torres Strait Islander people have significantly worse health, education, employment, and economic outcomes, compared to the rest of the Australian population.
In 2008 the Council of Australian Governments (COAG) created the National Indigenous Reform Agreement to close the gap between indigenous and non-indigenous Australians, listing six key targets:
- to close the life expectancy gap within a generation
- to halve the gap in mortality rates for Indigenous children under five within a decade
- to ensure access to early childhood education for all Indigenous four-year-olds in remote communities within five years
- to halve the gap in reading, writing and numeracy achievements for children within a decade
- to halve the gap for Indigenous students in year 12 attainment rates by 2020 and
- to halve the gap in employment outcomes between Indigenous and non-Indigenous Australians within a decade.
Progress against these and additional targets is reported to the Federal Parliament annually. Successive governments have committed to achieving equity, but the disparities remain dire. Closing the Gap data shows:
- If you are born an indigenous woman your life expectancy is 75.6 years, compared to 83.4 for non-indigenous women. If you are an Aboriginal male, your life expectancy is 71.6 years compared to 80.2 for non-indigenous men.
- In 2020, 94 per cent of non-indigenous babies are born with a healthy birthweight compared to 89 per cent of Aboriginal and Torres Strait Islander babies.
- Aboriginal and Torres Strait Islander people are massively over-represented in our jails (2151.1 per 100,000 adult population in 2022, versus 15.7 per 100,000 non-indigenous people). Former federal Opposition leader Bill Shorten has said: “A young Aboriginal man of 18 in Australia is more likely to end up in jail than university”, a statement subsequently verified by researchers.
- Aboriginal and Torres Strait Islander people are also more likely to have their children taken away (56.8 per 1000 children in out-of-home care in 2022 compared to 4.8 per 1000 for non-indigenous families). This is despite the Australian Human Rights Commission ‘Stolen Generations’ national enquiry, which handed down its findings in 1997.
- In 2018-19, 8.4 per cent of Aboriginal and Torres Strait Islander females aged 15 years and over experienced domestic physical or threatened physical harm.
- In 2021, 68.1 % of Aboriginal and Torres Strait Islander people aged 20-24 years had obtained a Year 12 or equivalent educational qualification, compared to 90.7 per cent of non-indigenous people aged 20-24.
Deaths in custody are not included within the Closing the Gap goals. There have been more than 500 indigenous deaths in custody since the Royal Commission into Aboriginal Deaths in Custody handed down its report in 1991. The report contained 339 recommendations, many of which have not been implemented.
Living by our values
MediRecords’ core values state that we “act with integrity, actively listening to clients and colleagues and striving to improve health care delivery for our community”. The Closing the Gap data indicates government policies are either not improving health outcomes – or not doing so fast enough.
We believe that empowering First Australians with the Voice to Parliament they have asked for is a way to enable more influence and input into policies that affect their lives. We support a “not about me, without me” approach to policy making.
This is why we will be voting, ’Yes.’
Referendum FAQS
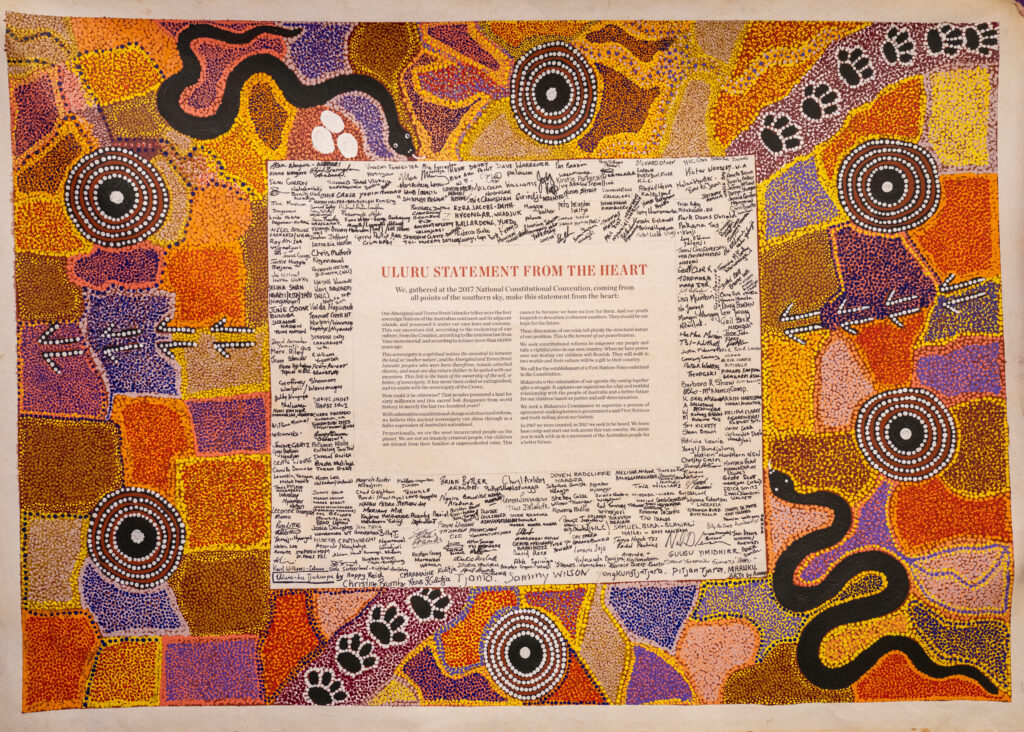
Aboriginal and Torres Strait Islander people want more say in the laws that affect them. In 2017, following consultations across Australia, the First Nations National Constitutional Convention delivered the powerful Uluru Statement from the Heart. One of the things the statement calls for is, “establishment of a First Nations Voice enshrined in the Constitution”. It also states: “We seek constitutional reforms to empower our people and take a rightful place in our own country. When we have power over our destiny our children will flourish. They will walk in two worlds and their culture will be a gift to their country.”
You can hear the full Uluru Statement, read by Indigenous community leaders, here:
https://youtu.be/rWoIgPyQTK4
The Australian Constitution is the primary set of rules that determine how Australia is governed. Our Constitution was introduced in 1901. The only way to update the Constitution is through a process known as a ‘referendum’. First, both houses of the Federal Parliament must endorse a change to the Constitution. A national vote is then held so the Australian people can say ‘yes’ or ‘no’ to the proposed change. A majority of voters in a majority of states and territories, AND a majority of voters nationally, must vote ‘yes’ for a referendum to succeed.
While most previous attempts to change the Constitution have been unsuccessful, one of the successful ‘yes’ votes also involved Aboriginal people. Before 1967, the Constitution did not even acknowledge Aboriginal and Torres Strait islander people were part of the Australian population. In the 1967 referendum, 91% of Australians, with a majority in every state or territory, voted to update the Constitution to include Aboriginal and Torres Strait Islander people as part of Australia’s population, and empower the Commonwealth Government to make laws affecting them.
The 2023 referendum is a vote on whether you support the Constitution being changed to establish a Voice to Parliament. You will be asked to answer ‘yes’ or ‘no’ to the following question:
“A Proposed Law: to alter the Constitution to recognise the First Peoples of Australia by establishing an Aboriginal and Torres Strait Islander Voice. Do you approve this proposed alteration?”
If successful, the following words will be added to the Constitution:
Chapter IX Recognition of Aboriginal and Torres Strait Islander Peoples
S 129 Aboriginal and Torres Strait Islander Voice
In recognition of Aboriginal and Torres Strait Islander peoples as the First Peoples of Australia:
1. There shall be a body, to be called the Aboriginal and Torres Strait Islander Voice;
2. The Aboriginal and Torres Strait Islander Voice may make representations to the Parliament and the Executive Government of the Commonwealth on matters relating to Aboriginal and Torres Strait Islander peoples;
3. The Parliament shall, subject to this Constitution, have power to make laws with respect to matters relating to the Aboriginal and Torres Strait Islander Voice, including its composition, functions, powers, and procedures.
As these words show, the proposed Voice does not give Aboriginal and Torres Strait Islander people the power to make, alter or block national laws. The Voice just gives Aboriginal and Torres Strait Islanders a presence in parliament to offer advice and feedback on policies, based on their lived experience.
The referendum on a Voice to parliament will take place on a date (yet to be announced,) between September and December this year. It is compulsory by law for all eligible Australian citizens aged 18 and older to enrol and vote in referendums.
The Australian Electoral Commission (AEC) has published information on the referendum, including Yes and No arguments, here: Your official referendum 2023 pamphlet (aec.gov.au) The AEC also has a Disinformation Register.
The following video discusses widespread misinformation on the Voice and is well worth watching: https://youtu.be/Nla61MfEtiY
Further learning
Archie Roach – ‘Took the Children away’: https://youtu.be/IL_DBNkkcSE
Challenging Terra Nullius | National Library of Australia (nla.gov.au)
It’s official — the Voice referendum is happening. Here’s what comes next – ABC News
Supporting the Voice makes for better health outcomes – WAPHA
The Voice Design Principles – Uluru Statement from the Heart
Together, Yes – First Nations Voice to parliament (togetheryes.com.au)
References
History of Closing the Gap | Closing the Gap
Fact check: Are young Indigenous men more likely to end up in jail than university? – ABC News
Bringing them home: The ‘Stolen Children’ report (1997) | Australian Human Rights Commission
Royal Commission into Aboriginal Deaths in Custody | naa.gov.au
Who We Are – our goal to improve the way healthcare is delivered (medirecords.com)
Voice to Parliament – Reconciliation Australia
Australian Constitution – Parliamentary Education Office (peo.gov.au)