March 23, 2023
MediRecords in the
fast lane for FHIR connectivity

MediRecords will be releasing new FHIR integration pathways for clients throughout 2023, as part of our commitment to a better connected Australian healthcare system.
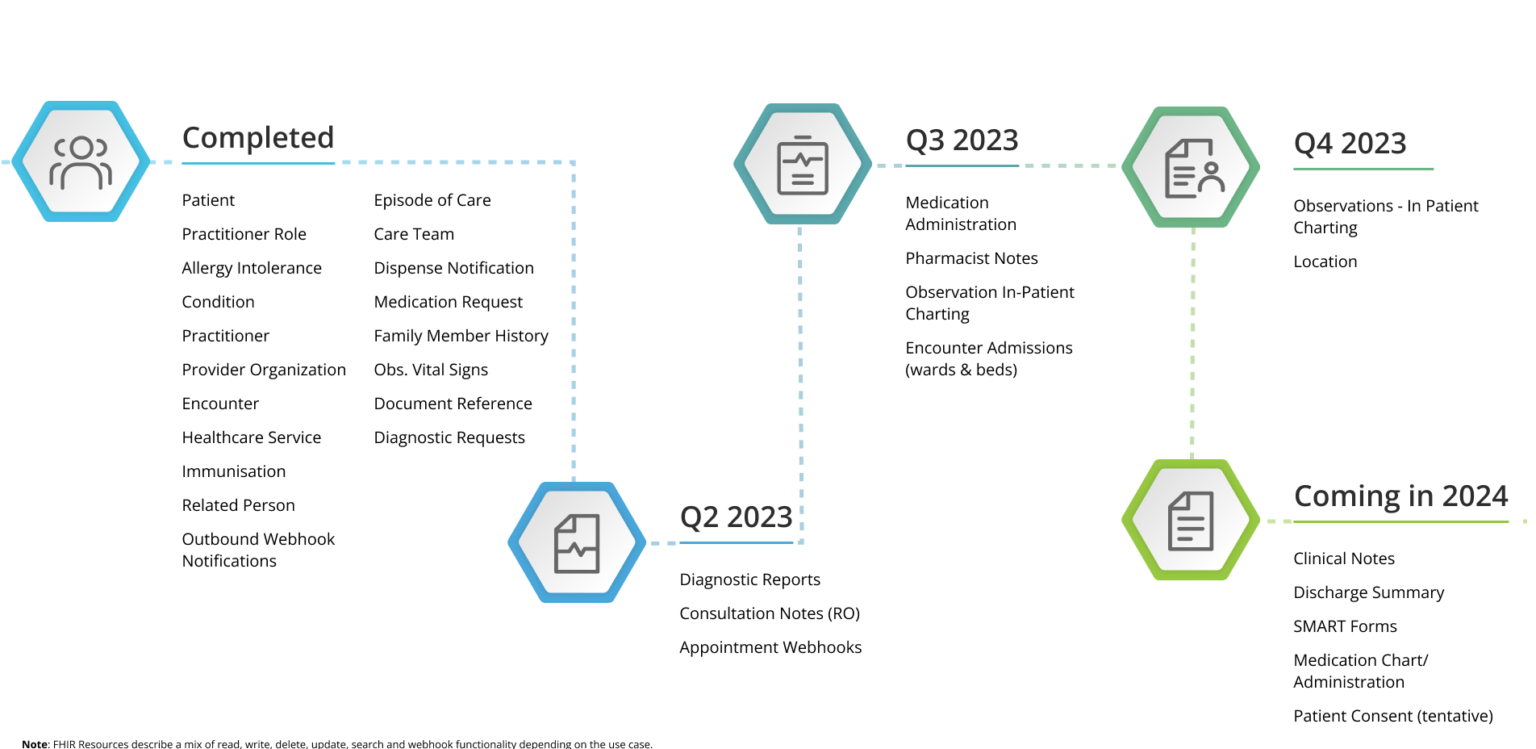
As can be seen from our FHIR Roadmap below, we not only have established and proven options for data sharing, but we’re investing in the expansion of our Connect platform which comprises of FHIR (Fast Health Interoperability Resources) and Connect services.
We now have FHIR integrations with hospital systems for ePrescribing, and updating patient records. New resources in development for MediRecords 2.0 include allergies, diagnostic requests and reports, patient summaries, and inpatient charting.
MediRecords Chief Executive Officer Matthew Galetto said the Connect platform enabled health care providers and patients to access records quickly and securely, driving better and timelier health outcomes.
“We’re keen to see more software vendors hit the road and deliver on industry standards for interoperability, resulting in connected health care across Australia,” Mr Galetto said.
“Some vendors seem to be waiting for a reason to modernise when the motivation should be clear — the right care at the right time, wherever you are in Australia.”
MediRecords is part of a national consortium, led by Leidos Australia, developing a new Health Knowledge Management (HKM) system for the Australian Defence Force. This project will see MediRecords connect health records for GPs, allied health practitioners, specialists, patients, and hospitals.
MediRecords is also supporting the Victorian Virtual Emergency Department with an integrated ePrescribing system.
MediRecords Technical Product Lead Sanjeed Quaiyumi said 2023 would be an exciting year. “We’re working on consultation notes and can’t wait to hit other milestones on our roadmap.”
MediRecords FHIR Roadmap
MediRecords FHIR roadmap was last updated 01/11/23.