May 01, 2024
MediRecords wises up
on CSIRO’s Smart Forms
for Healthcare

The initiative will see Smart Forms technology deployed in the MediRecords platform, enabling faster access to new clinical assessment tools and patient surveys.
The first Smart Form, a Falls Risk Assessment, is expected to be available in MediRecords this month.
Commissioned by the Commonwealth Department of Health, Smart Forms technology was developed to improve health assessment procedures and clinical information sharing, leading to better patient outcomes. This was first demonstrated through the Aboriginal and Torres Strait Islander Health Check Assessment Smart Form.
Standardised forms can streamline how clinicians capture patient data and simplify how this data is made available for research and other analysis.
MediRecords Integrations Lead Sanjeed Quaiyumi said Smart Forms would accelerate the introduction of new health assessments within MediRecords.
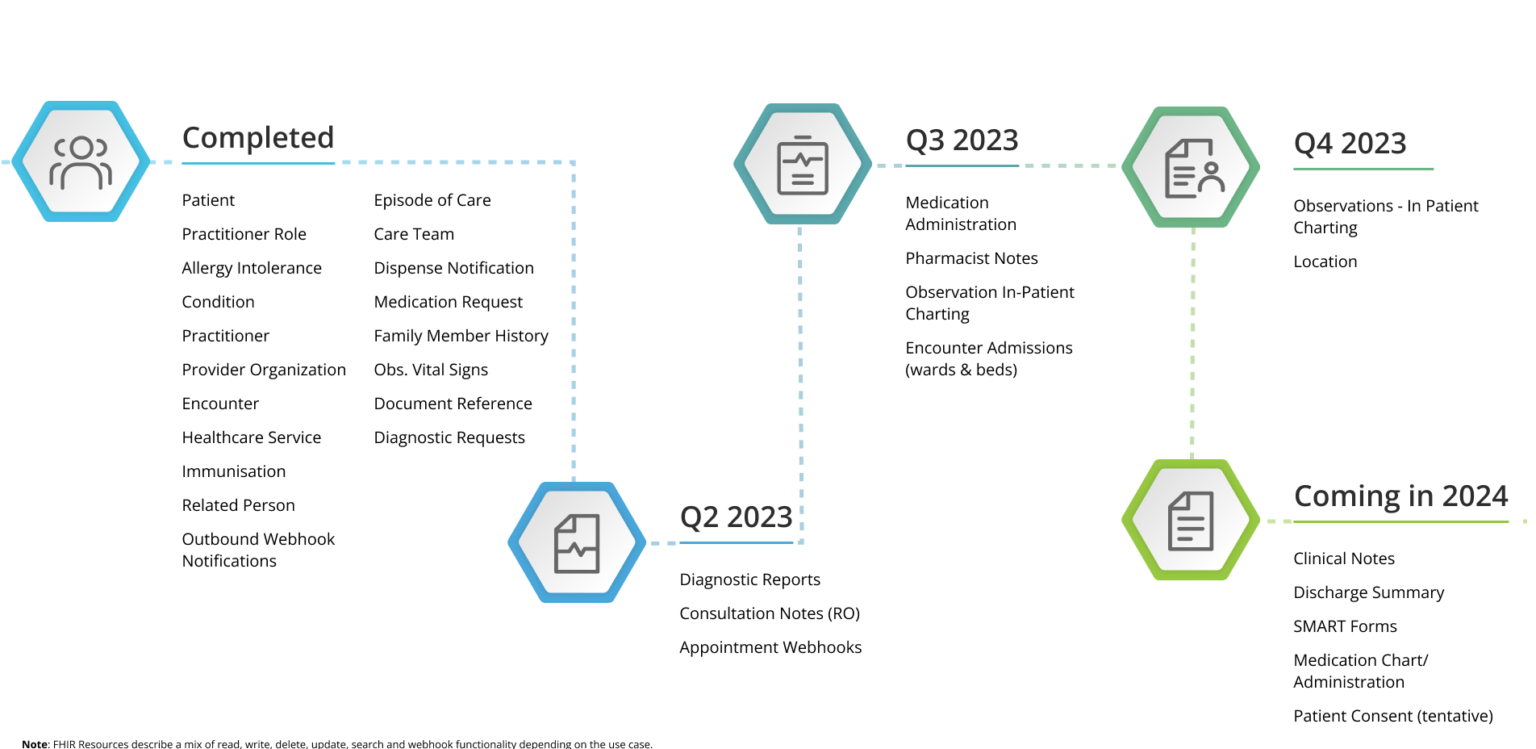
“MediRecords is laying the foundations for the adoption of Fast Healthcare Interoperability Resources (FHIR) in the broader health ecosystem, having developed and implemented an extensive library of FHIR and API resources. Smart Forms provide an exciting new way to gather and share data.”
What are Smart Forms?
Smart Forms conform to the HL7 FHIR Structured Data Capture and SMART App Launch Implementation Guides, ensuring seamless interoperability between clinical systems and applications. This standardised approach facilitates exchange of electronic health information across a diverse range of platforms.
Key benefits of Smart Forms include:
- Interoperability: Facilitating seamless data exchange between FHIR-enabled healthcare applications and systems
- Adaptability: Customisable forms tailored to specific clinical contexts and user needs
- Standardisation: Adherence to standardised data formats and coding conventions for consistency in healthcare data representation
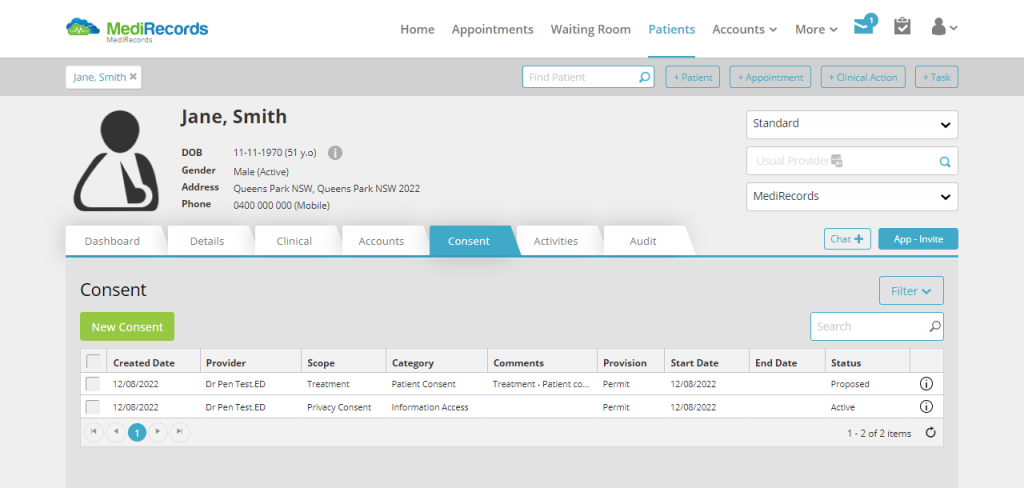
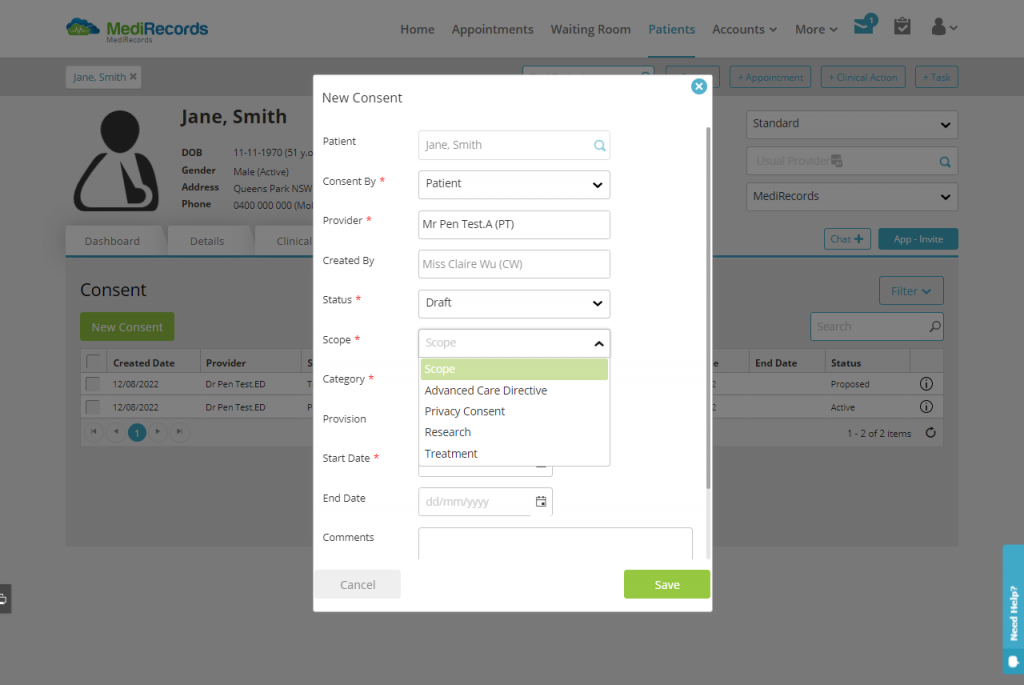
- Security: Robust security measures to safeguard patient data and maintain privacy
- User-Friendly Interface: Designed for accessibility across various levels of technical expertise
- Enhanced Workflow Efficiency: Streamlined data capture, retrieval, and exchange processes for improved decision-making and patient care coordination.
MediRecords will use Smart Forms to expand its range of clinical templates, starting with the Falls Risks Assessment and extending to inpatient Admissions and Primary Care Assessments forms.
This initiative underscores MediRecords’ commitment to driving innovation and enhancing healthcare outcomes through cutting-edge technologies. By harnessing the power of CSIRO’s Smart Forms, MediRecords aims to significantly improve data capture options, providing clinicians with advanced tools for delivering personalised patient care.
MediRecords actively participates in the Sparked FHIR Accelerator community. Sparked is a collaboration between Department of Health and Aged Care, the Australian Digital Health Agency, HL7 Australia and CSIRO’s Australian e-Health Research Centre.
Media inquiries:
For media inquiries or further information, please contact MediRecords Senior Business Development Manager Tim Pegler via tim.pegler@medirecords.com.
References:
Home – AU Core Implementation Guide v0.3.0-ballot (hl7.org.au)
https://aehrc.csiro.au/wp-content/uploads/2023/11/2022_23-AEHRC-Annual-Report.pdf