March 7, 2023
MediRecords 2.0: New ways to Care, Connect
and Engage
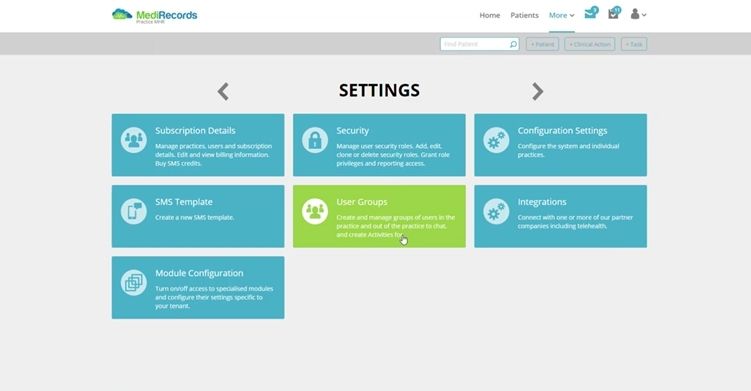
MediRecords 2.0 is the most comprehensive overhaul of our electronic patient record and clinic management system since we launched in Australia in 2016. While there have been many product updates over the years, MediRecords 2.0 is designed to use screen space better, streamline workflows, reduce administrative burn-out and support shared care.
MediRecords Head of Product Jayne Thompson says, “Innovation is as important to us as it is to our customers”. The 2.0 product update reflects this philosophy, introducing best-in-class user experience design and other client-driven enhancements, while reinforcing the foundations for next generation digital health connectivity.
Having grown beyond its origins as Australia’s pioneering, cloud-based practice management system, the MediRecords platform is now underpinned by three pillars: Care, Connect and Engage. Each of these will gain major new features during 2023.
Care
The MediRecords Care pillar contains core clinical features such as patient records, ePrescribing, appointment management, investigations, billing and claiming, correspondence, and assessments. New Care functionality will include:
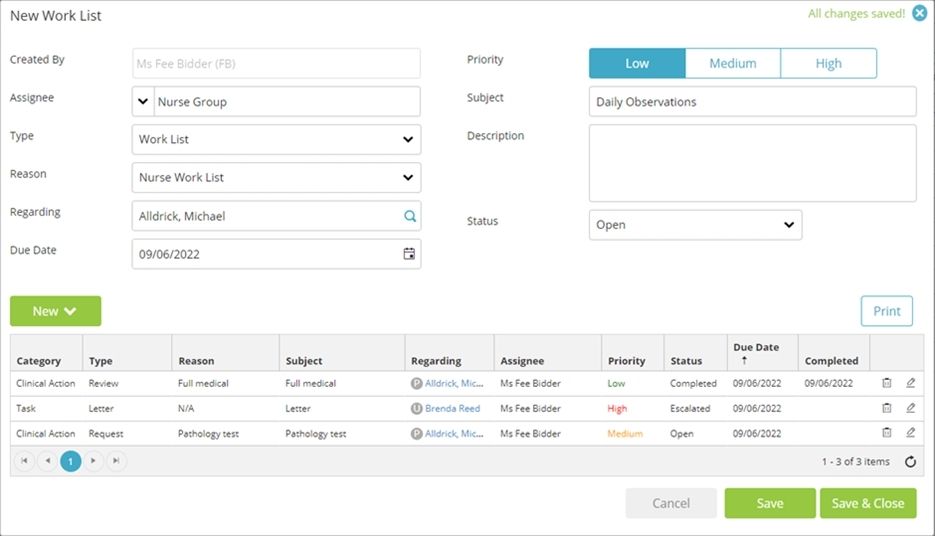
- Case Management – Members of a designated Care Team can view and update client case notes. This is particularly valuable where care is shared between a multidisciplinary team working from separate locations or across different shifts. For example, mental health practitioners can collaborate with GPs and rehabilitation specialists as patients progress towards a safe return to work.
- Group appointments – Patients will be able to book and join group sessions or classes. This feature will enable group therapy, family consultations and community health programs, with providers able to message an entire group or individual group members.
- New mental health and readiness for work assessment templates are being added, including the Glasgow Coma Scale.
- Single provider view of appointments: Clinicians practising across multiple clinics won’t have to jump between them to view their appointments. Appointments across multiple sites will be consolidated in a single view.
- New communication capability: Real time chat with team members will be available throughout MediRecords, making it easier to message team members on the fly. Our new Comms bar will also provide shortcuts to SMS, email, alerts, and notifications.
- Inpatients – In a major new premium* feature, MediRecords will be able to support complex care, including inpatient admissions, detailed charting, clinical escalations, progress notes and Discharge Summaries.
- Our Letter writer tool is having a makeover and will be even easier to use, with highly requested new functionality, such as digital signatures.
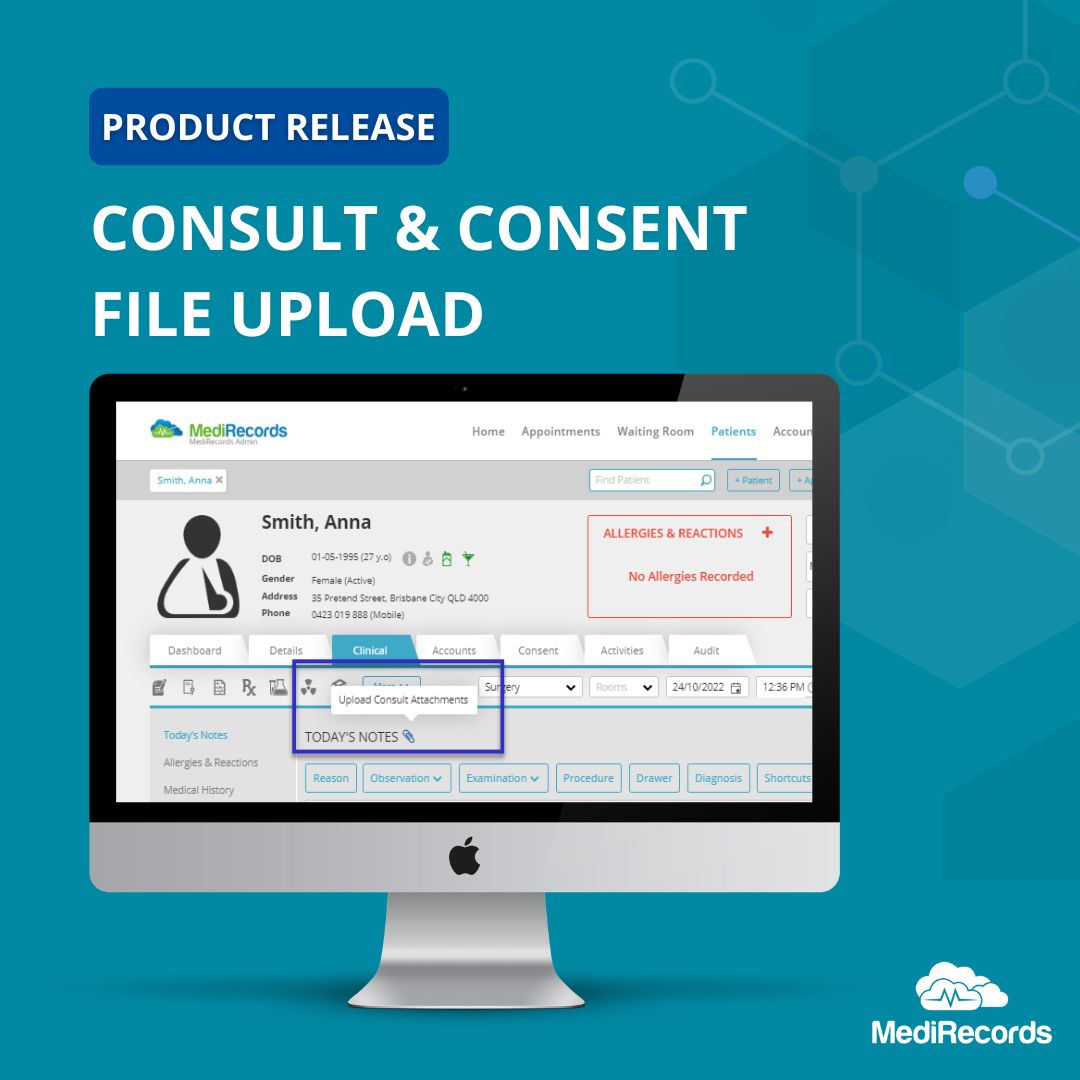
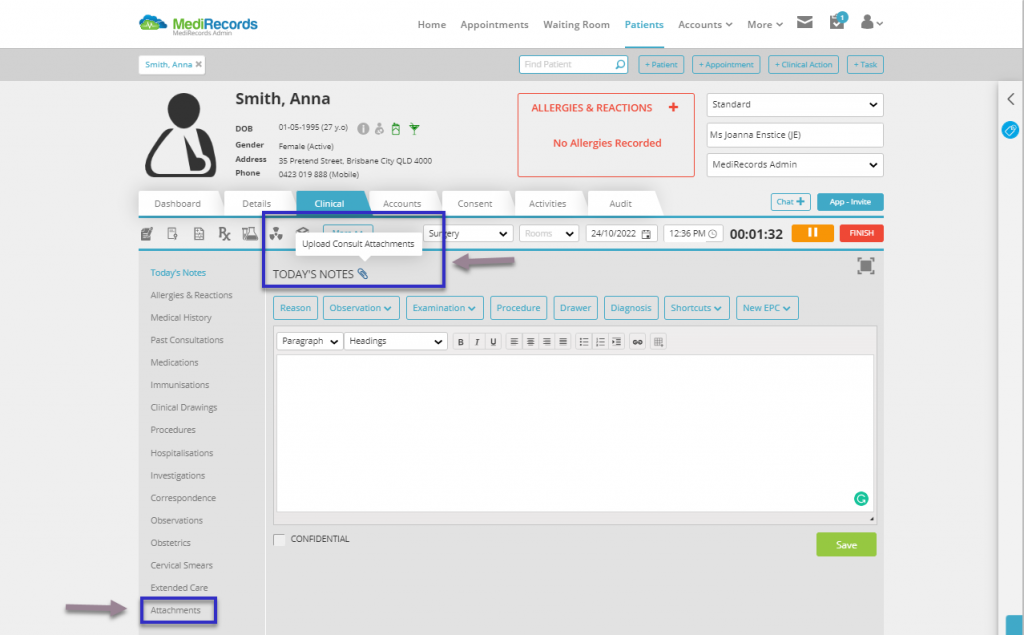
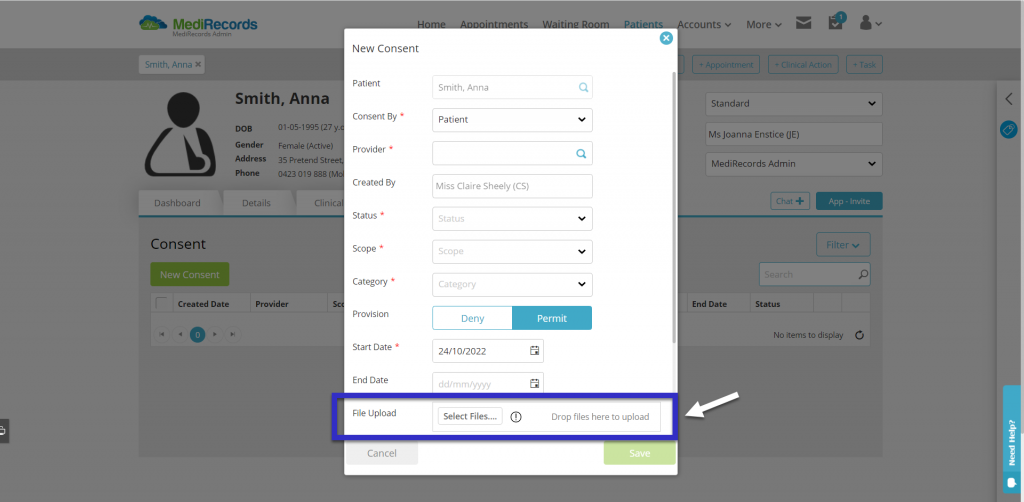
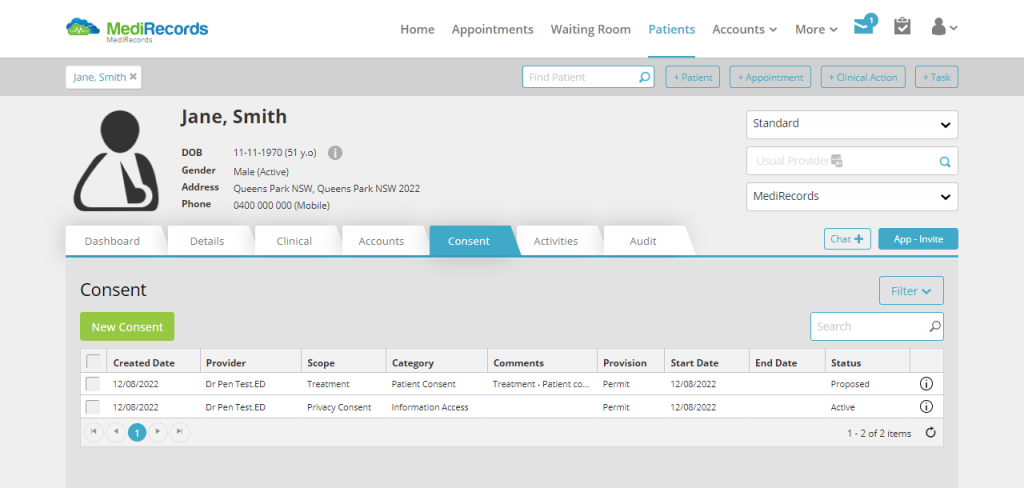
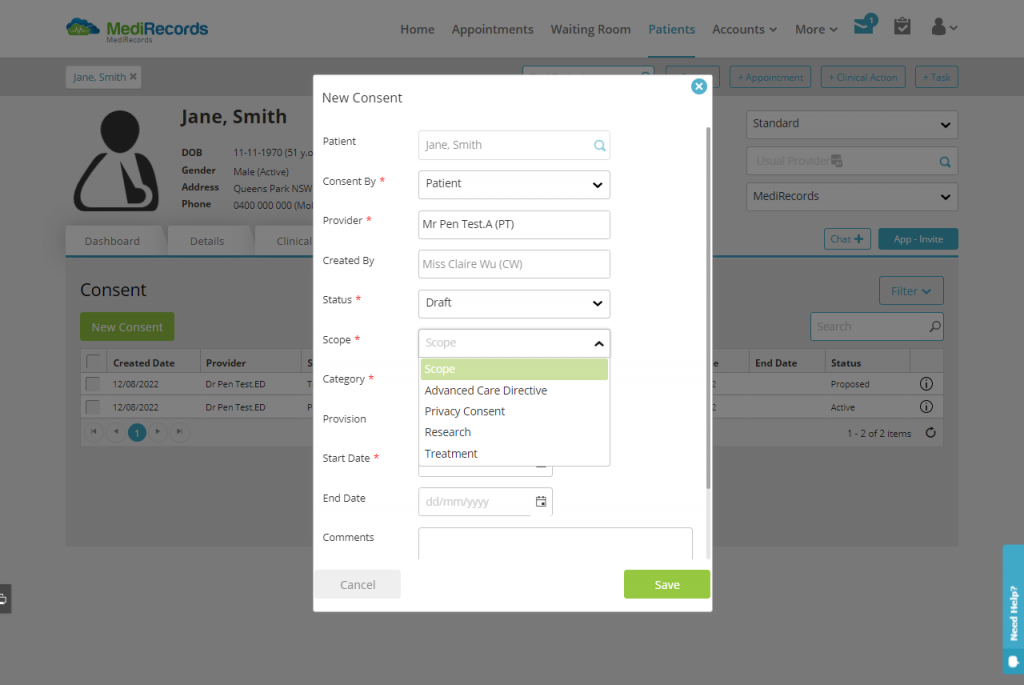
- We’ve added industry-leading means of recording Consent (or denial of consent) and made it easier to add attachments to patient records.
- Custom fields and Tagging can be used in patient records, creating new and innovative ways to capture information, search records and report on data.
Connect
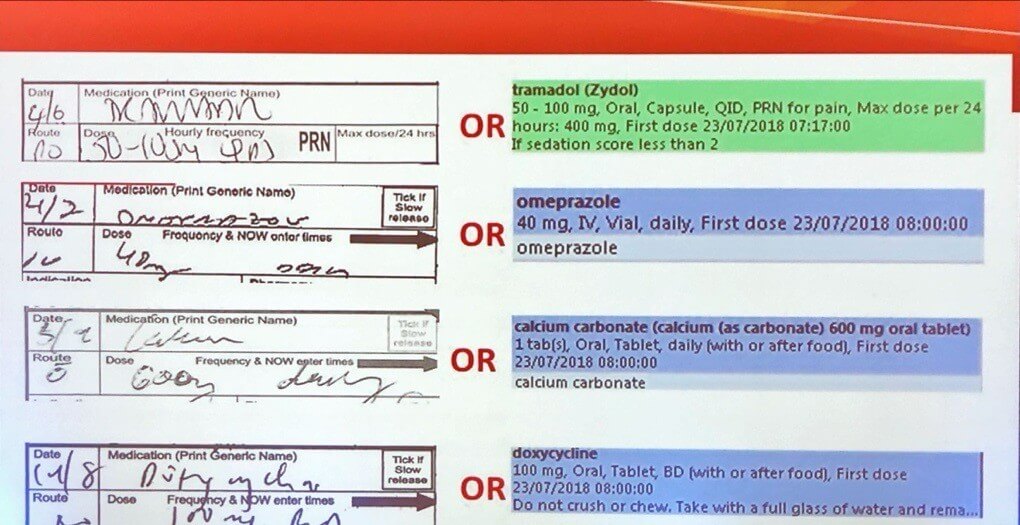
Many clients are familiar with our Connect site. MediRecords was an early adopter of FHIR (Fast Health Interoperability Resources) and API technology and new options for using these to share data are on the way. We have proven integrations with patient monitoring devices, patient-reported outcome and engagement measure systems (PROMs and PREMs), dictation technology and partner products. MediRecords is built on the SNOMED-CT-AU data coding system, which makes the data we share cleaner and primed for analytics.
- We now have FHIR integrations with enterprise products such as hospital patient administration systems (PAS) and scanned medical record software. This means a patient record created or updated in MediRecords can be pushed up into hospital systems, ensuring consistency of records and supporting better patient safety. Current options include allergies, medication requests and dispense notifications.
- New FHIR resources to be added throughout 2023 include referrals, diagnostic requests, diagnostic reports, and vital signs.
Engage
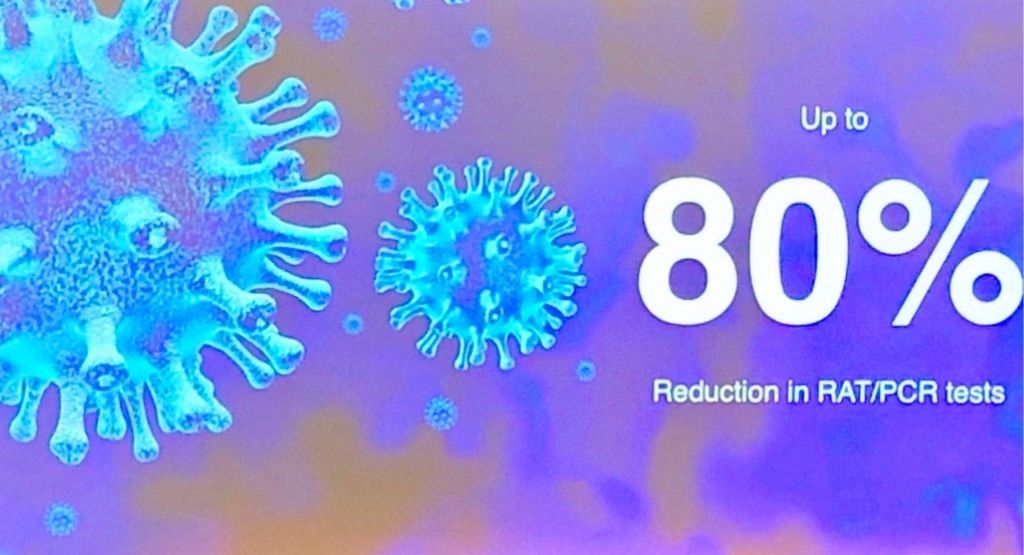
MediRecords has already connected over 60,000 patients to healthcare records via our patient mobile app. This enables consumers to book appointments, see medication information, receive reports and educational resources, and access and store personal health documents. We’re taking this to the next level in 2023 with an entirely new patient engagement platform. This will include new features such as:
- Real time surveys and forms
- Clinical assessment and observations data for remote monitoring
- In-appointment chat functionality
- Secure web access to personal health data.
Frequently asked questions
MediRecords 2.0 is an overhaul of our current platform rather than a new product. All existing customers will transition to 2.0. Sticking with the old MediRecords format will not be an option.
We will perform the update remotely. Users won’t have to download or do anything.
We have done our utmost to preserve familiarity and usual behaviour within the MediRecords application, but the new layout may take some adjustment. To help with this, we have been providing Lunch and Learn sessions for clients. Please reach out to our training team if you have any further questions, training.success@medirecords.com.
Development will finish in March. Rigorous testing will follow before pilot sites switch to 2.0 in late April. Once we have considered their feedback, we’ll finalise the date for general release and shout it from the rooftops to let you know.
If you are a current client, please contact your Account Manager if you would like to be a test pilot for these new features. Limited places are available.
MediRecords 2.0 is an upgrade of your existing system and will be covered by usual licence fees. However, some of the optional new features will be Premium products and require additional fees. Details will be published as soon as possible.
For other questions, please email support@medirecords.com.