August 30, 2024
Meditations on a National Conference with a conscience

The theme for the Catholic Health Australia National Conference that wound up in Sydney this week was ‘Rejoice Reimagine’. MediRecords has attended numerous innovation-focused gatherings over the years, but none where faith and belief have been so central to proceedings.
The theme for the Catholic Health Australia National Conference that wound up in Sydney this week was ‘Rejoice Reimagine’. MediRecords has attended numerous innovation-focused gatherings over the years, but none where faith and belief have been so central to proceedings. Here are four take-aways from the event.
Keynote speaker Dr Gill Hicks spoke with amazing grace about the events that led to her being critically wounded in a London terrorist attack and hospitalised for six months, initially labelled by rescuers as ‘one unknown, estimated female’. Dr Hicks said there is always opportunity in adversity; she used the loss of her legs as her chance to become taller, through longer than recommended prosthetic limbs. She said the thought of not being able to make a natural footprint on Australian soil had been confronting until she realised ‘how we leave each other’ is of more lasting importance.
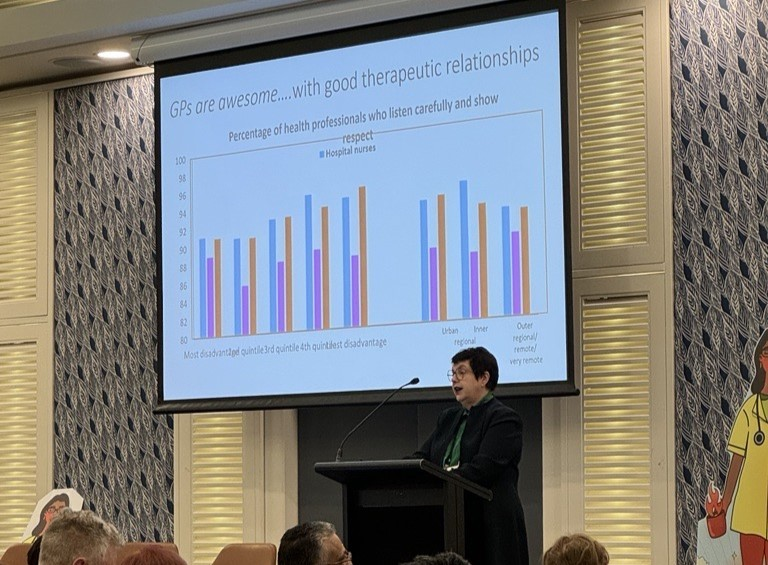
Australian Government Department of Health and Aged Care Secretary Blair Comley said that in developing a strategic map for health and aged care nationally, the department was aware it should be thinking 15 to 30 years ahead. He said the strategy had four key priorities:
- Prioritise prevention and early intervention.
- Address health and aged care inequities.
- Enhance system integration, in part through private sector engagement.
- Leverage available health and digital technology.
Australian Medical Association federal president Professor Steve Robson said the recent introduction of electronic medical record (EMR) technology that was non-intuitive and complex for users had been a catastrophe. The transition period had been “really awful”, and several senior colleagues had left healthcare due to added stress and workload. Professor Robson urged politicians to spend less time cutting ribbons and announcing tech projects, when the focus should be on systems that enable patient-centred care.
Operations Manager at St Vincent’s Health Network Sydney Katya Issa spoke of how prison accelerates aging and exacerbates existing illnesses. Older people often enter prison without medications, mobility aids and glasses, and can face long delays getting these. She said St Vincent’s Health needed to keep advocating for sentencing reform, age-specific facilities and more transitional services for people leaving prisons.
Senior Peer Worker at the NSW Justice Health & Forensic Mental Health Network, Andrew Padayachy, who was arrested, charged and then had all charges dropped after several months in prison, spoke of the humiliation of being wheeled into a public hospital for a brain scan, handcuffed by hands and feet to a wheelchair. Mr Padayachy also called for greater support for people being released as many had become dependent on the justice system, having forgotten how to live in the community.
MediRecords welcomes opportunities to work with faith-based and social justice organisations. An alternative to larger EMR vendors, our interoperable, secure, cloud-hosted Electronic Health Records system provides a longitudinal view of care in the community and hospitals. Our new Admissions module, built to support 200 beds managed by the Australian Defence Force, includes electronic prescribing, progress notes, handovers, charting, and assessments. Medication management and a new patient portal are in development.
MediRecords welcomes opportunities to work with faith-based and social justice organisations. An alternative to larger EMR vendors, our interoperable, secure, cloud-hosted Electronic Health Records system provides a longitudinal view of care in the community and hospitals. Our new Admissions module, built to support 200 beds managed by the Australian Defence Force, includes electronic prescribing, progress notes, handovers, charting, and assessments. Medication management and a new patient portal are in development.